Androgen insensitivity syndrome
Definition
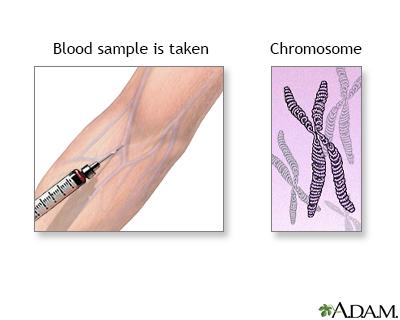
Androgen insensitivity syndrome (AIS) is when a person who is genetically male (who has one X and one Y chromosome) is resistant to male hormones (called androgens). As a result, the person has some of the physical traits of a woman, but the genetic makeup of a man.
Alternative Names
Testicular feminization
Causes
AIS is caused by genetic defects on the X chromosome. These defects make the body unable to respond to the hormones that produce a male appearance.
The syndrome is divided into two main categories:
- Complete AIS
- Partial AIS
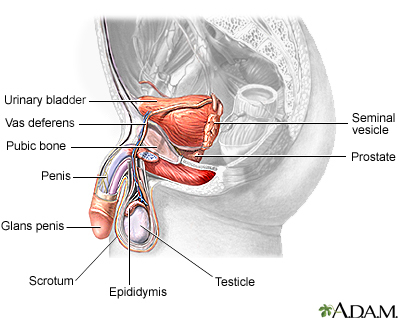
In complete AIS, the penis and other male body parts fail to develop. At birth, the child looks like a girl. The complete form of the syndrome occurs in as many as 1 in 20,000 live births.
In partial AIS, people have different numbers of male traits.
Partial AIS can include other disorders, such as:
- Failure of one or both testes to descend into the scrotum after birth
- Hypospadias, a condition in which the opening of the urethra is on the underside of the penis, instead of at the tip
- Reifenstein syndrome (also known as Gilbert-Dreyfus syndrome or Lubs syndrome)
Infertile male syndrome is also considered to be part of partial AIS.
Symptoms
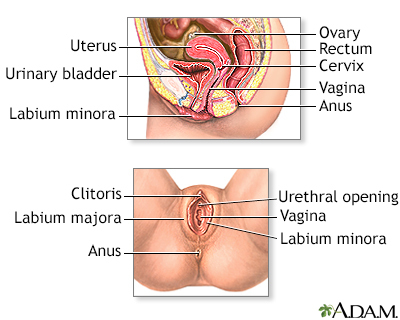
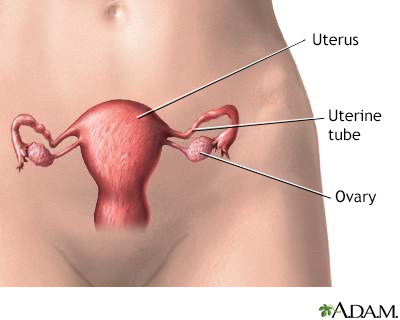
A person with complete AIS appears to be female but has no uterus. They have very little armpit and pubic hair. At puberty, female sex characteristics (such as breasts) develop. However, the person does not menstruate and become fertile.
People with partial AIS may have both male and female physical characteristics. Many have partial closing of the outer vagina, an enlarged clitoris, and a short vagina.
There may be:
- A vagina but no cervix or uterus
- Inguinal hernia with testes that can be felt during a physical exam
- Normal female breasts
- Testes in the abdomen or other atypical places in the body
Exams and Tests
Complete AIS is rarely discovered during childhood. Sometimes, a growth is felt in the abdomen or groin that turns out to be a testicle when it is explored with surgery. Most people with this condition are not diagnosed until they do not get a menstrual period or they have trouble getting pregnant.
Partial AIS is often discovered during childhood because the person may have both male and female physical traits.
Tests used to diagnose this condition may include:
- Blood tests to check levels of testosterone, luteinizing hormone (LH), and follicle-stimulating hormone (FSH)
- Genetic testing (karyotype) to determine the person's genetic makeup
- Pelvic ultrasound
Other blood tests may be done to help tell the difference between AIS and androgen deficiency.
Treatment
Testicles that are in the wrong place may not be removed until a child finishes growing and goes through puberty. At this time, the testes may be removed because they can develop cancer, just like any undescended testicle.
Estrogen replacement may be prescribed after puberty.
Treatment and gender assignment can be a very complex issue, and must be targeted to each individual person.
Outlook (Prognosis)
The outlook for complete AIS is good if the testicle tissue is removed at the right time to prevent cancer.
Possible Complications
Complications include:
- Infertility
- Psychological and social issues
- Testicular cancer
When to Contact a Medical Professional
Contact your health care provider if you or your child has signs or symptoms of the syndrome.
Gallery
References
Chan Y-M, Hannema SE, Achermann JC, Hughes IA. Disorders of sex development. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 24.
Donohoue PA. Disorders of sex development. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 606.
Yu RN, Diamond DA. Disorders of sexual development: etiology, evaluation, and medical management. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 48.