Understanding Trigeminal Neuralgia: Symptoms, Causes and Treatment Options
Trigeminal neuralgia is a challenging condition that can cause excruciating pain in the face.
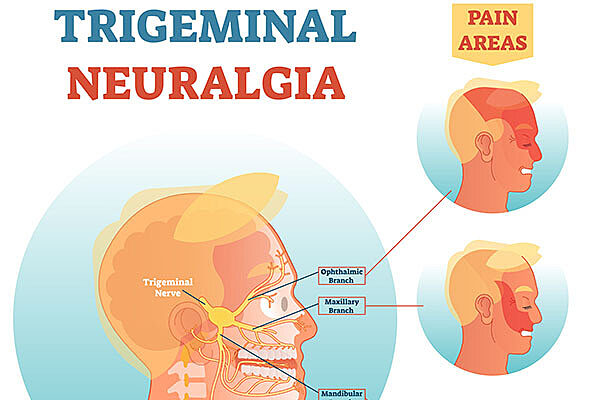
The condition affects the trigeminal nerve, which is responsible for transmitting sensation from the face to the brain, leading to severe pain on one side of the face that can be triggered by the slightest touch or movement.
The condition is not life-threatening and can be managed with proper treatment.
Along with trigeminal neuralgia expert William Friedman, MD, a professor in the department of neurosurgery at the University of Florida, we will provide information and resources for those who are living with this condition.
We will also offer guidance for loved ones who may be seeking ways to support someone who is suffering from trigeminal neuralgia.
What are the symptoms of trigeminal neuralgia?
The pain associated with trigeminal neuralgia is often described as a sharp, shooting or electric shock-like sensation that lasts anywhere from a few seconds to minutes. The pain can be triggered by many things, such as:
- Applying makeup
- Brushing your teeth
- Drinking
- Eating
- Shaving
- Talking
- Touching your face
- Wind or air on your face
Trigeminal neuralgia pain can be so severe that it interferes with daily activities, like eating, talking and sleeping.
What causes trigeminal neuralgia?
Trigeminal neuralgia is usually caused by a small blood vessel pulsating against the trigeminal nerve. Patients with multiple sclerosis can develop trigeminal neuralgia without vascular compression.
In rare cases, the compression is caused by a tumor.
What are the treatment options for trigeminal neuralgia?
The treatment for trigeminal neuralgia depends on the severity of the pain and the underlying cause. The preferred treatment is a medication called carbamazepine.
“Surgery is reserved for those cases where medication fails to control pain or causes intolerable side effects,” Dr. Friedman said.
Help is out there
Living with trigeminal neuralgia can be challenging, but with proper treatment, most patients can be cured. If you or someone you know is experiencing symptoms of trigeminal neuralgia, it is important to seek medical attention.
Frequently Asked Questions About Trigeminal Neuralgia
How is trigeminal neuralgia diagnosed?
A doctor can diagnose trigeminal neuralgia by reviewing your medical history and symptoms and performing a physical exam. Imaging tests such as an MRI may be ordered to rule out other conditions that also cause facial pain.
“Trigeminal neuralgia is often diagnosed incorrectly. It can be confused with dental problems, headache syndromes, temporal arteritis, sinusitis and tumors of the brain or the face,” Dr. Friedman said.
What is the trigeminal nerve?
The trigeminal nerve is responsible for sending sensation signals from the face to the brain. In people with trigeminal neuralgia, this nerve can become irritated or compressed, causing intense pain.
How is trigeminal neuralgia treated?
Treatment for trigeminal neuralgia often includes medication to help manage the pain. Some people may also benefit from surgery to decompress the nerve or destroy part of it.
Does trigeminal neuralgia show on an MRI?
An MRI can help confirm trigeminal neuralgia as it shows whether the nerve is being compressed by surrounding blood vessels or other structures. It can help confirm if surgery is the right option.
What does trigeminal neuralgia pain feel like?
The pain is described as sudden, sharp, stabbing pain that can last from a few seconds to several minutes. It is usually felt on one side of the face and can be triggered by things like touching the face, brushing teeth or even a gust of wind.
Can you live a normal life with trigeminal neuralgia?
While trigeminal neuralgia can be difficult to live with, most patients can find relief with proper treatment.
