Byssinosis
Definition
Byssinosis is a disease of the lungs. It is caused by breathing in cotton dust or dusts from other vegetable fibers such as flax, hemp, or sisal while at work.
Alternative Names
Cotton worker's lung; Cotton bract disease; Mill fever; Brown lung disease; Monday fever
Causes
Breathing in (inhaling) the dust produced by raw cotton can cause byssinosis. It is most common in people who work in the textile industry.
Those who are sensitive to the dust can have an asthma-like condition after being exposed.
Methods of prevention in the United States have reduced the number of cases. Byssinosis is still common in developing countries. Smoking increases risk of developing this disease. Being exposed to the dust many times can lead to long-term (chronic) lung disease.
Symptoms
Symptoms may include any of the following:
- Chest tightness
- Cough
- Wheezing
- Shortness of breath
Symptoms are worse at the beginning of the work week and improve later in the week. Symptoms are also less severe when the person is away from the workplace.
Exams and Tests
Your health care provider will take a detailed medical history. You'll be asked whether your symptoms relate to certain exposures or times of exposure. The provider will also do a physical exam, paying special attention to the lungs.
Tests that may be ordered include:
Treatment
The most important treatment is to stop being exposed to the dust. Reducing dust levels in the factory (by improving machinery or ventilation) will help prevent byssinosis. Some people may have to change jobs to avoid further exposure.
Medicines used for asthma, such as bronchodilators, usually improve symptoms. Corticosteroid drugs may be prescribed in more severe cases.
Stopping smoking is very important for people with this condition. Breathing treatments, including nebulizers, may be prescribed if the condition becomes long-term. Home oxygen therapy may be needed if blood oxygen level is low.
Physical exercise programs, breathing exercises, and patient education programs are often helpful for people with a long-term (chronic) lung disease.
Outlook (Prognosis)
Symptoms usually improve after stopping exposure to the dust. Continued exposure can lead to reduced lung function. In the United States, worker's compensation may be available to people with byssinosis.
Possible Complications
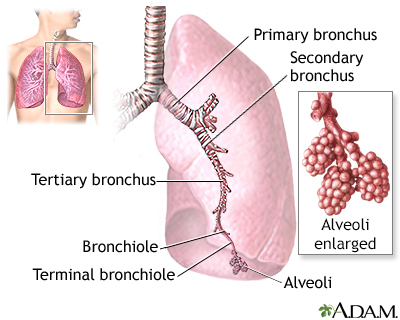
Chronic bronchitis may develop. This is swelling (inflammation) of the large airways of the lungs with a large amount of phlegm production.
When to Contact a Medical Professional
Call your provider if you have symptoms of byssinosis and exposure to cotton or other fibers.
Call your provider if you suspect that you have been exposed to cotton or other fiber dust at work and you have breathing problems. Having byssinosis makes it easier for you to develop lung infections.
Talk to your provider about getting the flu and pneumonia vaccines.
If you've been diagnosed with byssinosis, call your provider right away if you develop a cough, shortness of breath, fever, or other signs of a lung infection, especially if you think you have the flu. Since your lungs are already damaged, it's very important to have the infection treated right away. This will prevent breathing problems from becoming severe. It will also prevent further damage to your lungs.
Prevention
Controlling dust, using face masks, and other measures can reduce the risk. Stop smoking, especially if you work in textile manufacturing.
Gallery
References
Go LHT, Cohen RA. Pneumoconioses. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 101.
Tarlo SM. Occupational lung disease. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 87.