Chylomicronemia syndrome
Definition
Chylomicronemia syndrome is a disorder in which the body does not break down fats (lipids) correctly. This causes fat particles called chylomicrons to build up in the blood. The disorder is passed down through families.
Alternative Names
Familial lipoprotein lipase deficiency; Familial hyperchylomicronemia syndrome, Type I hyperlipidemia
Causes
Chylomicronemia syndrome can occur due to a rare genetic disorder in which a protein (enzyme) called lipoprotein lipase (LpL) is broken or missing. It can also be caused by the absence of second factor called apo C-II, which activates LpL. LpL is normally found in fat and muscle. It helps break down certain lipids. When LpL is missing or broken, fat particles called chylomicrons build up in the blood. This buildup is called chylomicronemia.
Defects in apolipoprotein CII and apolipoprotein AV can cause the syndrome as well. It is more likely to occur when people who are predisposed to have high triglycerides (such as those who have familial combined hyperlipidemia or familial hypertriglyceridemia) develop diabetes, obesity or are exposed to certain medicines.
Symptoms
Symptoms may start in infancy and include:
- Abdominal pain due to pancreatitis (inflammation of the pancreas).
- Symptoms of nerve damage, such as loss of feeling in the feet or legs, and memory loss.
- Yellow deposits of fatty material in the skin called xanthomas. These growths may appear on the back, buttocks, soles of the feet, or ankles, knees and elbows.
Exams and Tests
A physical exam and tests may show:
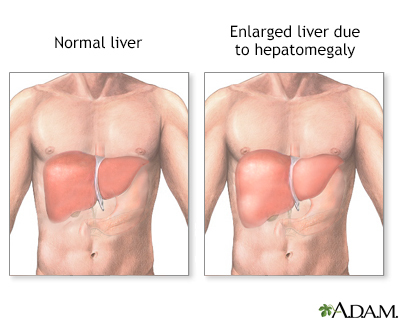
- Enlarged liver and spleen
- Inflammation of the pancreas
- Fatty deposits under the skin
- Possibly fatty deposits in the retina of the eye
A creamy layer will appear when blood spins in a laboratory machine. This layer is due to chylomicrons in the blood.
The triglyceride level is extremely high.
Treatment
A fat-free, alcohol-free diet is required. You may need to stop taking certain medicines that can make symptoms worse. Do not stop taking any medicine without first talking to your health care provider. Conditions such as dehydration and diabetes can make symptoms worse. If diagnosed, these conditions need to be treated and controlled.
Outlook (Prognosis)
A fat-free diet can reduce symptoms dramatically.
Possible Complications
When untreated, the excess chylomicrons may lead to bouts of pancreatitis. This condition can be very painful and even life threatening.
When to Contact a Medical Professional
Seek medical care right away if you have abdominal pain or other warning signs of pancreatitis.
Contact your provider if you have a personal or family history of high triglyceride levels.
Prevention
There is no way to prevent someone from inheriting this syndrome.
Gallery

References
Genest J, Mora S, Libby P. Lipoprotein disorders and cardiovascular disease. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 27.
Robinson JG. Disorders of lipid metabolism. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 195.