Definition
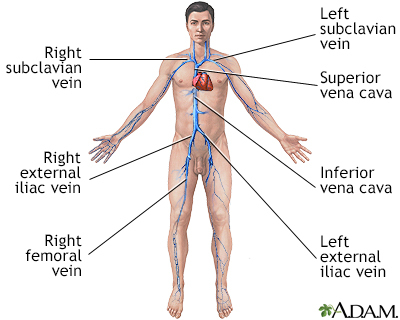
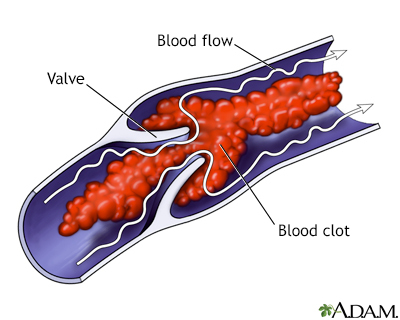
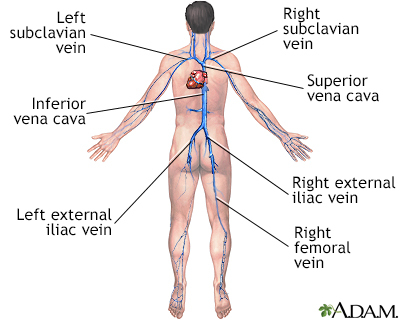
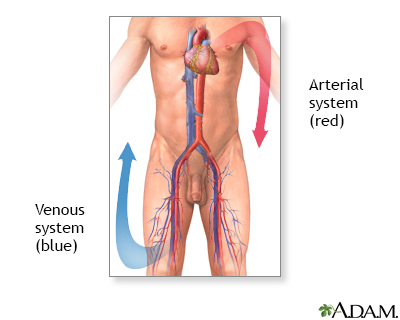
Deep vein thrombosis (DVT) is a condition that occurs when a blood clot forms in a vein deep inside a part of the body. It mainly affects the large veins in the lower leg and thigh, but can occur in other deep veins, such as in the arms and pelvis.
Alternative Names
DVT; Blood clot in the legs; Thromboembolism; Post-phlebitic syndrome; Post-thrombotic syndrome; Venous - DVT
Causes
DVT is most common in adults over age 60. But it can occur at any age. When a clot breaks off and moves through the bloodstream, it is called an embolism. An embolism can get stuck in the blood vessels in the brain, lungs, heart, or another area, leading to severe damage.
Blood clots may form when something slows or changes the flow of blood in the veins. Risk factors include:
- A pacemaker catheter that has been passed through the vein in the groin
- Bed rest or sitting in one position for too long, such as plane travel
- Family history of blood clots
- Fractures in the pelvis or legs
- Giving birth within the last 6 months
- Pregnancy
- Obesity
- Recent surgery (most commonly hip, knee, or female pelvic surgery)
- Too many blood cells being made by the bone marrow, causing the blood to be thicker than normal (polycythemia vera)
- Having an indwelling (long-term) catheter in a blood vessel
Blood is more likely to clot in someone who has certain problems or disorders, such as:
- Cancer
- Certain autoimmune disorders, such as lupus
- Cigarette smoking
- Conditions that make it more likely to develop blood clots
- Taking estrogens or birth control pills (this risk is even higher with smoking)
Sitting for long periods when traveling can increase the risk for DVT. This is most likely when you also have one or more of the risk factors listed above.
Symptoms
DVT mainly affects the large veins in the lower leg and thigh, most often on one side of the body. The clot can block blood flow and cause:
- Changes in skin color (redness)
- Leg pain
- Leg swelling (edema)
- Skin that feels warm to the touch
Exams and Tests
Your health care provider will perform a physical exam. The exam may show a red, swollen, or tender leg.
The two tests that are often done first to diagnose a DVT are:
A pelvic MRI may be done if the blood clot is in the pelvis, such as after pregnancy.
Blood tests may be done to check if you have an increased chance of blood clotting, including:
- Activated protein C resistance (checks for the Factor V Leiden mutation)
- Antithrombin III levels
- Antiphospholipid antibodies
- Complete blood count (CBC)
- Genetic testing to look for mutations that make you more likely to develop blood clots, such as the prothrombin G20210A mutation
- Lupus anticoagulant
- Protein C and protein S levels
Treatment
Your provider will give you medicine to thin your blood (called an anticoagulant). This will keep more clots from forming or old ones from getting bigger.
Heparin is often the first medicine you will receive.
- If heparin is given through a vein (IV), you must stay in the hospital. However, most people can be treated without staying in the hospital.
- Low molecular weight heparin can be given by injection under your skin once or twice a day. You may not need to stay in the hospital as long, or at all, if you are prescribed this type of heparin.
One type of blood-thinning medicine called warfarin (Coumadin or Jantoven) may be started along with heparin. Warfarin is taken by mouth. It takes several days to fully work.
Another class of blood thinners works differently than warfarin. Examples of this class of medicines, called direct oral anticoagulants (DOAC), include:
- Rivaroxaban (Xarelto)
- Apixaban (Eliquis)
- Dabigatran (Pradaxa)
- Edoxaban (Savaysa)
These drugs work in a similar way to heparin and can be used right away in place of heparin. Your provider will decide which medicine is right for you.
You will most likely take a blood thinner for at least 3 months. Some people take it longer, or even for the rest of their lives, depending on their risk for another clot.
When you are taking a blood thinning medicine, you are more likely to bleed, even from activities you have always done. If you are taking a blood thinner at home:
- Take the medicine just the way your provider prescribed it.
- Ask the provider what to do if you miss a dose.
- Get blood tests as advised by your provider to make sure you are taking the right dose. These tests are usually needed with people who are taking warfarin.
- Learn how to take other medicines and when to eat.
- Find out how to watch for problems caused by the medicine.
In rare cases, you may need surgery instead of or in addition to anticoagulants. Surgery may involve:
- Placing a filter in the body's largest vein to prevent blood clots from traveling to the lungs
- Removing a large blood clot from the vein or injecting clot-busting medicines
Follow any other instructions you are given to treat your DVT.
Outlook (Prognosis)
DVT often goes away without a problem, but the condition can return. The symptoms can appear right away or you may not develop them for 1 or more years afterward. Wearing compression stockings during and after the DVT may help prevent this problem.
Possible Complications
Complications of DVT may include:
- Fatal pulmonary embolism (blood clots in the thigh are more likely to break off and travel to the lungs than blood clots in the lower leg or other parts of the body)
- Constant pain and swelling (post-phlebitic or post-thrombotic syndrome)
- Varicose veins
- Non-healing ulcers (less common)
- Changes in skin color
When to Contact a Medical Professional
Contact your provider if you have symptoms of DVT.
Go to the emergency room or call the local emergency number (such as 911) if you have DVT and you develop:
References
Kabrhel C. Pulmonary embolism and deep vein thrombosis. In: Walls RM, Hockberger RS, Gausche-Hill M, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 74.
Lockhart ME, Umphrey HR, Weber TM, Robbin ML. Peripheral vessels. In: Rumack CM, Levine D, eds. Diagnostic Ultrasound. 5th ed. Philadelphia, PA: Elsevier; 2018:chap 27.
Siegal D, Lim W. Venous thromboembolism. In: Hoffman R, Benz EJ, Silberstein LE, et al, eds. Hematology: Basic Principles and Practice. 7th ed. Philadelphia, PA: Elsevier; 2018:chap 142.
Stevens SM, Woller SC, Kreuziger LB, et al. Antithrombotic therapy for VTE disease: second update of the CHEST guideline and expert panel report. Chest. 2021 Dec;160(6):e545-e608. Epub 2021 Aug 2. PMID: 34352278. https://pubmed.ncbi.nlm.nih.gov/34352278/.