Emergency contraception
Definition
Emergency contraception is a birth control method to prevent pregnancy in women. It can be used:
- After a sexual assault or rape
- When a condom breaks or a diaphragm slips out of place
- When a woman forgets to take birth control pills
- When you have sex and do not use any birth control
- When any method of birth control is not used correctly
Alternative Names
Morning-after pill; Postcoital contraception; Birth control - emergency; Plan B; Family planning - emergency contraception
Information
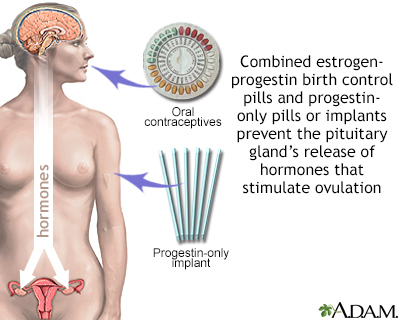
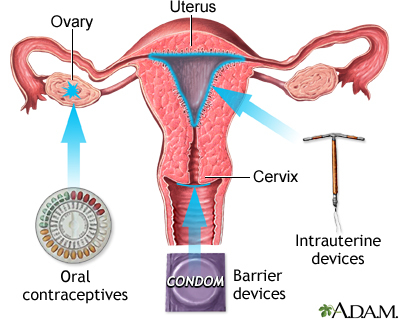
Emergency contraception most likely prevents pregnancy in the same way as regular birth control pills:
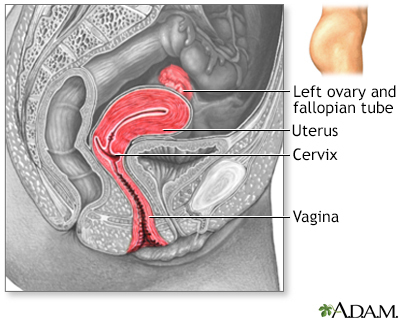
- By preventing or delaying the release of an egg from a woman's ovaries
- By preventing the sperm from fertilizing the egg
The two ways you may receive emergency contraception are by:
- Using pills that contain a man-made (synthetic) form of the hormone progesterone called progestins. This is the most common method.
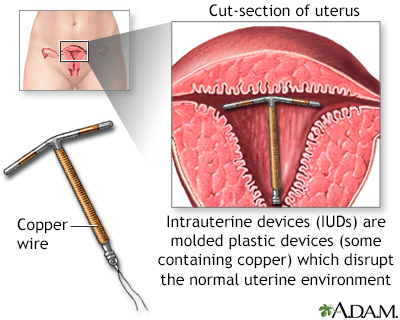
- Having an IUD placed inside the uterus.
CHOICES FOR EMERGENCY CONTRACEPTION
Two emergency contraceptive pills may be bought without a prescription.
- Plan B One-Step is a single tablet.
- Next Choice is taken as 2 doses. Both pills can be taken at the same time or as 2 separate doses 12 hours apart.
- Either may be taken for up to 5 days after unprotected intercourse.
Ulipristal acetate (Ella) is a new type of emergency contraception pill. You will need a prescription from a health care provider.
- Ulipristal is taken as a single tablet.
- It may be taken up to 5 days after unprotected sex.
Birth control pills may also be used:
- Talk to your provider about the correct dosage.
- In general, you must take 2 to 5 birth control pills at the same time to have the same protection.
IUD placement is another option:
- It must be inserted by your provider within 5 days of having unprotected sex. The IUD that is used contains a small amount of copper.
- Your doctor can remove it after your next period. You may also choose to leave it in place to provide ongoing birth control.
MORE ABOUT EMERGENCY CONTRACEPTIVE PILLS
Women of any age can buy Plan B One-Step and Next Choice at a pharmacy without a prescription or visit to a health care provider.
Emergency contraception works best when you use it within 24 hours of having sex. However, it may still prevent pregnancy for up to 5 days after you first had sex.
You should not use emergency contraception if:
- You think you have been pregnant for several days.
- You have vaginal bleeding for an unknown reason (talk to your provider first).
Emergency contraception may cause side effects. Most are mild. They may include:
- Changes in menstrual bleeding
- Fatigue
- Headache
- Nausea and vomiting
After you use emergency contraception, your next menstrual cycle may start earlier or later than usual. Your menstrual flow may be lighter or heavier than usual.
- Most women get their next period within 7 days of the expected date.
- If you do not get your period within 3 weeks after taking emergency contraception, you might be pregnant. Contact your provider.
Sometimes, emergency contraception does not work. However, research suggests that emergency contraceptives have no long-term effects on the pregnancy or developing baby.
OTHER IMPORTANT FACTS
You may be able to use emergency contraception even if you cannot regularly take birth control pills. Talk to your provider about your options.
Emergency contraception should not be used as a routine birth control method. It does not work as well as most types of birth control.
Gallery
References
Allen RH, Kaunitz AM, Hickey M, Brennan A. Hormonal contraception. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 18.
Rivlin K, Davis AR. Contraception and abortion. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 13.
Winikoff B, Grossman D. Contraception. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 225.