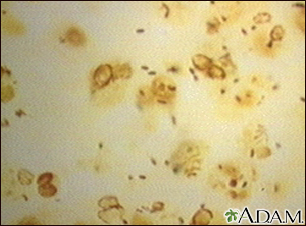
Legionnaire disease
Definition
Legionnaire disease is an infection of the lungs and airways. It is caused by Legionella bacteria.
Alternative Names
Legionella pneumonia; Pontiac fever; Legionellosis; Legionella pneumophila
Causes
The bacteria that cause Legionnaire disease have been found in water delivery systems. They can survive in the warm, moist air conditioning systems of large buildings, including hospitals.
Most cases are caused by the bacteria Legionella pneumophila. The rest of the cases are caused by other Legionella species.
Spread of the bacteria from person to person has not been proven.
Most infections occur in middle-aged or older people. In rare cases, children can get the infection. When they do, the disease is less severe.
Risk factors include:
- Alcohol use
- Cigarette smoking
- Chronic illnesses, such as kidney failure or diabetes
- Long-term (chronic) lung disease, such as COPD
- Long-term use of a breathing machine (ventilator)
- Medicines that suppress the immune system, including chemotherapy and steroid drugs
- Older age
Symptoms
Symptoms tend to get worse during the first 4 to 6 days. They most often improve in another 4 to 5 days.
Symptoms may include:
- General discomfort, loss of energy, or ill feeling (malaise)
- Headache
- Fever, shaking chills
- Joint pain, muscle aches and stiffness
- Chest pain, shortness of breath
- Cough that does not produce much sputum or mucus (dry cough)
- Coughing up blood (rare)
- Diarrhea, nausea, vomiting, and abdominal pain
Exams and Tests
The health care provider will perform a physical exam. Abnormal sounds, called crackles, may be heard when listening to the chest with a stethoscope.
Tests that may be done include:
- Arterial blood gases
- Blood cultures to identify the bacteria
- Bronchoscopy to view the airways and diagnose lung disease
- Chest x-ray or CT scan
- Complete blood count (CBC), including white blood cell count
- ESR (sed rate) to check how much inflammation is in the body
- Liver blood tests
- Tests and cultures on sputum to identify the legionella bacteria
- Urine tests to check for Legionella pneumophila bacteria
- Molecular tests with polymerase chain reaction (PCR)
Treatment
Antibiotics are used to fight the infection. Treatment is started as soon as Legionnaire disease is suspected, without waiting for results of any lab test.
Other treatments may include receiving:
- Fluids through a vein (IV)
- Oxygen, which is given through a mask or breathing machine
- Medicines that are breathed in to ease breathing
Outlook (Prognosis)
Legionnaire disease can be life threatening. The risk of dying is higher in people who:
- Have long-term (chronic) diseases
- Become infected while in the hospital
- Are older adults
When to Contact a Medical Professional
Contact your provider right away if you have any type of breathing problem and think you have symptoms of Legionnaire disease.
Gallery
References
Edelstein PH, Roy CR. Legionnaires' disease and Pontiac fever. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 232.
Marrie TJ. Legionella infections. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 298.