Depression can be identified using gut bacteria, University of Florida Health researchers find
There’s a new ally in the effort to help people living with depression: gut bacteria. People with depression have distinct intestinal microbes that differ from those without the disorder, University of Florida Health researchers have found. That discovery has the potential to lead to new methods of diagnosing and treating depression using genetic profiling of gut bacteria, according to lead researcher Bruce R. Stevens, Ph.D., a professor in the UF College of Medicine’s department of physiology and functional genomics, and the department of medicine’s division of gastroenterology. Stevens further explains the findings, which were published Jan. 27 in Nature Molecular Psychiatry. Visit https://go.nature.com/2Sthlmg to see the report.
What are your main findings?
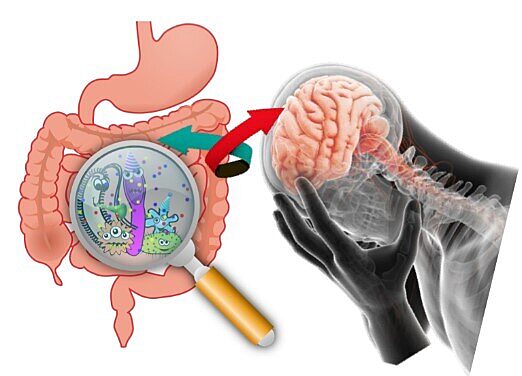
We had an idea that depression is an inflammation-based disorder involving certain regions of the brain. Our hypothesis was that gut bacteria can affect whole-body inflammation, brain inflammation and brain neurotransmitters — all of which can play a role in depression. To test that, we identified people living with depression and compared their gut bacteria with those who are in a healthy mental state. We found that we could identify and predict accurately if an individual is living with depression or had a healthy mental state based on their gut microbes. We do that by identifying the species of bacteria and the biochemicals from those bacteria that are relevant to depression.
How was the research conducted?
Microbial DNA in stool samples was obtained from research participants with a median age of 34 years old. Half of those people met the criteria for major depressive disorder, and half were mentally healthy people who served as control subjects for the research. To analyze and sort the massive amount of data we had to invent a novel machine-learning computer algorithm — a form of artificial intelligence.
Why use gut bacteria to diagnose depression?
We know that people’s bodies are made up of more than just human cells. Through evolution, we are actually an assemblage of trillions of human cells harboring and interacting with an equal number of microbes. Within this self-contained “meta-organism” ecosystem, our microbes and their genes serve as a type of add-on organ system. Conventional psychiatric analysis is based on behavioral interpretation by an experienced clinician. There is no medical test to diagnose depression. However, we know there is a three-way communication between gut bacteria, the body’s organ physiology and mood centers in the brain. So we knew that an objective technique like this would be useful to supplement a clinician’s subjective interpretation of depression. Our approach takes millions of data points about the nature of gut bacteria in people living with depression. It makes statistical decisions about whether that data are useful or irrelevant. Then it provides an easily comprehensible answer about the most prevalent gut bacteria and their molecules that interact with the brain’s mood centers. That gut bacteria profile is distinctive and identifiable among people living with depression.
Is this solely a diagnostic tool, or does it also have therapeutic potential?
It could be used for diagnosis but could also be used in the future for prevention or treatment. For example, we know that certain bacteria are responsive to particular antibiotics. That raises the possibility that antibiotics could be developed to target the gut microbiome of people living with depression. Certain antidepressants also have antibiotic properties, so there is the potential for them to be repurposed to target depression-related gut bacteria. Diet modification has therapeutic potential because types of food influence whether the gut harbors “good” or “bad” microbes. Also, a probiotic mix of select “antidepressant bacteria” is being explored.
What is the most novel aspect of these findings?
Our research redirects the future of psychiatry by implicating the gastrointestinal tract as a major target for diagnosis, treatment or prevention of depression. We used machine learning — a powerful computer-aided analysis that can be run on a supercomputer — to take massive amounts of data and distill it into a comprehensible analysis of gut bacteria composition and their biochemical signatures. It shows with substantial confidence that there is a way to identify people living with depression. Our findings suggests certain bacterial species of depression or resilience against depression may run in families. This may be due to unavoidably exchanging and retaining certain microbes by communal exposures steered by cultural settings such as food choices, hygiene or antibiotic overuse.
What is next for this research?
We are looking at other disorders that accompany depression and one of those is treatment-resistant hypertension (high blood pressure). Many people with hypertension are also depressed, so that arena is another of our ongoing microbiome projects.
About the author
