UF Health researchers develop app to help monitor new moms for postpartum complications
Obstetricians know many new mothers won’t come in for a doctor’s visit in the first four to six weeks after giving birth, a crucial period when they are susceptible to postpartum complications like high blood pressure and depression.
The COVID-19 pandemic hasn’t made it any easier.
“The earlier we can communicate with women and check in with them to see if anything is going on, the better we can identify problems and intervene so that symptoms don’t become significant,” said Kay Roussos-Ross, M.D., an associate professor in the University of Florida College of Medicine’s department of obstetrics and gynecology, part of UF Health, the university’s academic health center.
Roussos-Ross and colleagues responded to this challenge by developing a smartphone app called Gator MOMitor™ that new mothers can use to report worrying symptoms in the early weeks after giving birth. UF Health follows up with a phone call if someone reports a problem. The app was developed with the assistance of a grant of more than $190,000 from the Florida Department of Health.
Roussos-Ross said the American College of Obstetricians and Gynecologists, or ACOG, recommends that women be seen by a physician in the first one to three weeks after delivery.
The app launched in November, and so far about 100 UF Health patients have agreed to download it and participate in this pilot program. Roussos-Ross said the goal is to have 500 women take part. Each receives a $30 stipend.
Besides depression and high blood pressure disorders such as preeclampsia, the app helps women who have had a Cesarean delivery report symptoms of infection and those with diabetes to report problematic blood sugar levels.
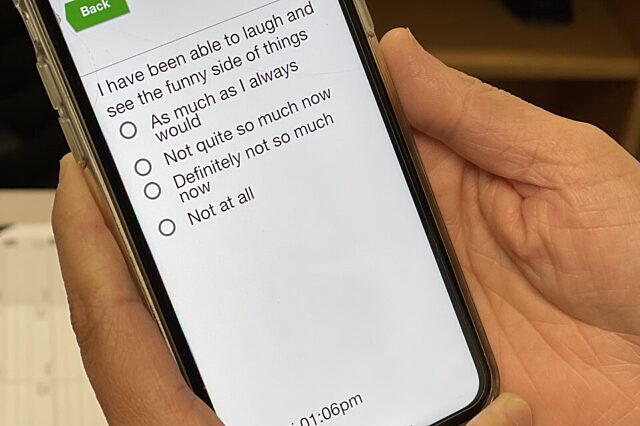
The app provides an easy-to-use format. Users are asked questions that apply to their treatment. To monitor for depression, for example, they are asked a series of questions about their mood. If they report being sad, they are asked additional questions. For example, they are asked for a response to the statement, “I have been able to laugh and see the funny side of things.” Responses include, “not at all” or “as much as I always would,” among others.
The responses are scored, with the app alerting the patient’s medical team if a follow-up call is warranted. If needed, a telehealth or in person appointment might be scheduled.
Women are also provided a blood pressure cuff, and if they report via the app that their pressure exceeds 140/90 mmHg, a nurse will follow up with a phone call.
“We’ll discuss what’s going on,” Roussos-Ross said. “Our hope with this app is to improve communication between the postpartum patient and her health team, allowing us to take better care of our patients and in turn decrease maternal morbidity. We want women to know that we are still invested in their health, even after the baby is delivered.”
Women with diabetes can use the app to report a blood sugar level above 200 mg/dL, which will prompt a similar call. Or those who have had a Cesarean delivery can even text a photo of their wound if it looks suspicious for infection.
Roussos-Ross noted that she and her colleagues have thought for quite some time about ways to monitor women for depression in the weeks after delivery. But the COVID-19 pandemic really brought home the urgency to find innovative ways to keep a postpartum connection between mother and health provider, Roussos-Ross said.
As part of the pilot project, participants will be asked for their feedback about the app and how well it worked, and whether they think the app would help other women.
The hope is that the app might eventually be expanded to encompass prenatal care.
The UF Health app uses a platform created by illumivu, an Asheville, North Carolina company that specializes in the development of health care apps connecting patients with their medical providers.
“We hope that our patients find it helpful,” Roussos-Ross said. “It’s crucial that we find ways to keep in touch with these new moms during the postpartum period, especially when a pandemic limits access to care. Technology can help us maintain that important connection.”
Media contact: Ken Garcia at kdgarcia@ufl.edu or 352-265-9408
About the author
