UF to lead national trial testing nerve block to alleviate headache from subarachnoid hemorrhage
A multidisciplinary team of neurocritical care, neurosurgery and pain medicine investigators from the University of Florida has been awarded a $12.9 million National Institutes of Health grant to test a novel way to relieve pain from sudden, excruciating headaches stemming from a burst brain aneurysm that causes bleeding.
The UF Health team will lead a 12-site national clinical trial this fall to test a nerve block procedure as an alternative to opioid medications to treat severe headaches caused by subarachnoid hemorrhage, a type of bleeding that irritates the lining of the brain after an aneurysm ruptures. This nerve block procedure already is commonly used at UF Health for pain relief from complex facial surgeries in adults and children and to treat other headache disorders, such as migraines.
Combining expertise from neurology, neurocritical care, neurosurgery, anesthesia and acute and perioperative pain medicine, the team is poised to run the first interventional therapeutic trial for headaches in subarachnoid hemorrhage and neurocritical care.
Called BLOCK-SAH, the 195-participant, double-blind four-year trial will assess the efficacy and safety of the nerve block procedure for severe headaches in subarachnoid hemorrhage and evaluate how well patients tolerate it. The procedure involves injecting a mix of a local anesthetic and a steroid through the edge of the temple and into the pterygopalatine fossa (pronounced TARE-ree-go-PAL-uh-teen FAUH-suh), a cone-shaped space holding the nerve structures where the pain originates.
The principal investigators at UF have assembled a team of collaborators that includes groups at Massachusetts General Hospital for clinical coordination and New York University for data management.
“Nearly everyone who is awake after suffering this condition complains of the most severe headache of their life; they say it hits them out of the blue, like a ‘thunderclap,’ and it is intolerable,” said Katharina M. Busl, M.D., M.S., a UF Health neurointensivist, chief of the division of neurocritical care and the trial’s lead principal investigator. “The headache currently is insufficiently treated with what we have available. Our idea was to find something outside the box that we could offer and that doesn’t come with all the side effects of opioids, such as blunting consciousness and sleepiness, and potentially long-term effects including addiction and rebound headaches. Our goal is to treat the pain from a mechanistically different angle.”
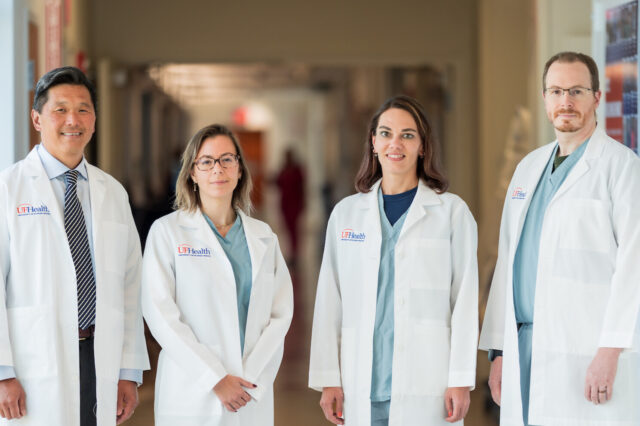
To do so, she has teamed up with fellow UF College of Medicine principal investigators Carolina B. Maciel, M.D., MSCR, a neurointensivist;Brian Hoh, M.D., M.B.A., chair of neurosurgery; and Cameron R. Smith, M.D., Ph.D., an acute pain medicine anesthesiologist who first started performing the pterygopalatine fossa block procedure in 2016 in infants, for painful cleft palate repair surgeries.
“It hurts enough that these babies refuse to eat for days,” Smith said. “The first pterygopalatine fossa block I did was on a 3-month-old baby, and when he woke up, he was surprisingly calm, and within an hour he was nursing.”
Since then, Smith has begun performing the procedure for other conditions, including sinus surgeries, tonsillectomies and headache disorders, including migraines.
To perform the nerve block, Smith inserts an ultra-thin 25-gauge needle into the edge of the temple, and the needle reaches about 5 centimeters to a space at the skull base where there are nerves responsible for many important functions, including conveying pain sensation in the head. For the patient, the insertion feels like a pinch and pressure, similar to an IV placement, he said. The injection delivers a mix of a local anesthetic, such as commonly used ropivacaine, and the steroid dexamethasone. Case series the team published in 2021 and 2022 found no significant complications from the procedure.
For the upcoming clinical trial, Smith and the procedural co-investigators will perform the nerve block using real-time ultrasound to ensure proper placement.
“Adult patients who are in the acute phase of subarachnoid hemorrhage following a ruptured aneurysm will have the option to participate in the trial after the aneurysm is treated,” Hoh said.
Those who enroll will receive two injections, one on each side of the head, on consecutive days, with randomized groups receiving either the anesthetic-steroid combination or a placebo saline injection. Then on the third and fourth days, all participants — including those in the placebo group — will have the option to receive injections with the active medications.
To begin rehabilitation from the injury, neurocritical care doctors encourage patients to get out of bed and regain mobility, such as spending time in a chair and walking laps around the unit. But the degree of pain or the lethargy from opioids can hinder recovery.
“When patients are in horrible pain, how can we expect them to heal and focus on their recovery journey? They barely have enough energy to eat, can’t sleep, can hardly move,” Maciel said. “From the hallway of the Neuro ICU, you can identify who is a subarachnoid hemorrhage patient because the room is dark and the door is closed.”
The researchers said their greatest hope is to bring relief.
“When you are healing from an acute brain injury, the energy needs to be focused on healing,” Busl said. “For these patients, the energy is really focused on just tolerating this relentless pain. It takes an unimaginable toll.”
“So what we want,” said Maciel, “is to be able to bring relief so they can actually carry on in their journey toward recovery.”
About the author
