Iron deficiency anemia
Definition
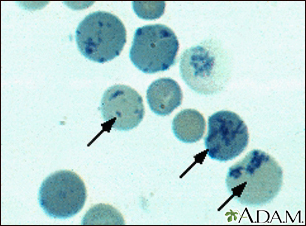
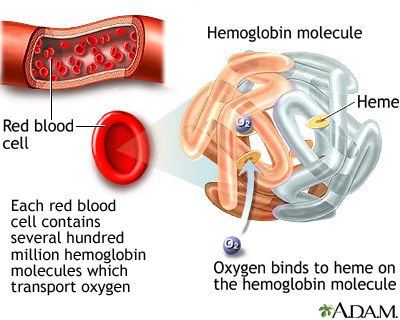
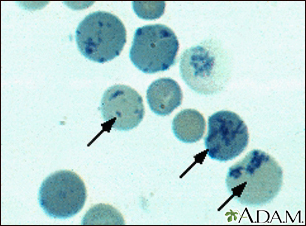
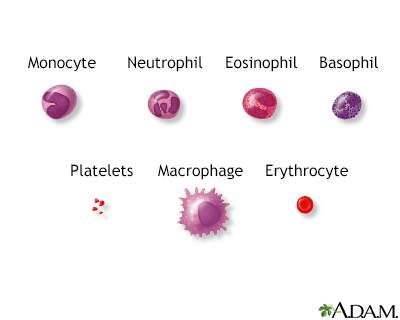
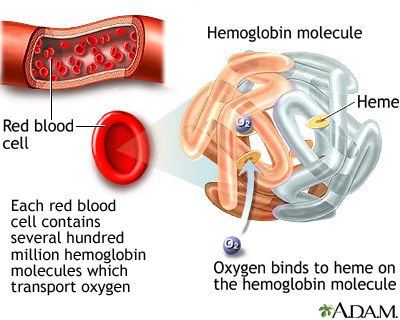
Anemia is a condition in which the body does not have enough healthy red blood cells. Red blood cells provide oxygen to body tissues. There are many types of anemia.
Iron deficiency anemia occurs when your body does not have enough iron. Iron helps make red blood cells. Iron deficiency anemia is the most common form of anemia.
Alternative Names
Anemia - iron deficiency
Causes
Patient Education Video: Iron deficiency anemia
Red blood cells bring oxygen to the body's tissues. Healthy red blood cells are made in your bone marrow. Red blood cells circulate through your body for 3 to 4 months. Parts of your body, such as your spleen, remove old blood cells.
Iron is a key part of red blood cells. Without iron, the blood cannot carry oxygen effectively. Your body normally gets iron through your diet. It also reuses iron from old red blood cells.
Iron deficiency anemia develops when your body's iron stores run low. This can occur because:
- You lose more blood cells and iron than your body can replace
- Your body does not do a good job of absorbing iron
- Your body is able to absorb iron, but you are not eating enough foods that contain iron
- Your body needs more iron than normal (such as if you are pregnant or breastfeeding)
Bleeding can cause iron loss. Common causes of bleeding are:
- Heavy, long, or frequent menstrual periods
- Cancer in the esophagus, stomach, small bowel, or colon
- Esophageal varices, often from cirrhosis
- The use of aspirin, ibuprofen, or arthritis medicines for a long time, which can cause gastrointestinal bleeding
- Peptic ulcer disease
The body may not absorb enough iron in your diet due to:
- Celiac disease
- Crohn disease
- Gastric bypass surgery
- Taking too many antacids or too much of the antibiotic tetracycline
You may not get enough iron in your diet if:
- You are a strict vegetarian
- You do not eat enough foods that contain iron
Symptoms
You may have no symptoms if the anemia is mild.
Most of the time, symptoms are mild at first and develop slowly. Symptoms may include:
- Feeling weak or tired more often than usual, or with exercise
- Headaches
- Dizziness
- Palpitations
- Problems concentrating or thinking
As the anemia gets worse, symptoms may include:
- Brittle nails
- Blue color to the whites of the eye
- Desire to eat ice or other non-food things (pica)
- Feeling lightheaded when you stand up
- Pale skin color
- Shortness of breath
- Sore or inflamed tongue
- Mouth ulcers
- Uncontrolled movement of legs (during sleep)
- Hair loss
Symptoms of the conditions (associated with bleeding) that cause iron deficiency anemia include:
- Dark, tar-colored stools or blood in the stool
- Heavy menstrual bleeding (women)
- Pain in the upper belly (from ulcers)
Exams and Tests
To diagnose anemia, your health care provider may order these blood tests:
- Complete blood count
- Reticulocyte count
To check iron levels, your provider may order:
- Bone marrow biopsy (if the diagnosis is not clear)
- Iron binding capacity (TIBC) in the blood
- Serum ferritin
- Serum iron level
To check for causes (blood loss) of iron deficiency, your provider may order:
- Colonoscopy
- Fecal occult blood test
- Upper endoscopy
- Tests to detect sources of blood loss in the urinary tract or uterus
Treatment
Treatment may include taking iron supplements and eating iron-rich foods.
Iron supplements (most often ferrous sulfate) build up the iron stores in your body. Most of the time, your provider will measure your iron level before you start supplements.
If you cannot take iron by mouth, you may need to take it through a vein (intravenous) or by an injection into the muscle.
Pregnant and breastfeeding women will need to take extra iron because they often cannot get enough iron from their normal diet.
Often your hematocrit should return to normal within 6 weeks of iron therapy. You will need to keep taking iron for another 6 to 12 months to replace the body's iron stores in the bone marrow.
Iron supplements are mostly well tolerated, but may cause:
- Nausea
- Vomiting
- Constipation
Iron-rich foods include:
- Chicken and turkey
- Dried lentils, peas, and beans
- Fish
- Meats (liver is the highest source)
- Soybeans, baked beans, chickpeas
- Whole-grain bread
Other sources include:
- Oatmeal
- Raisins, prunes, apricots, and peanuts
- Spinach, kale, and other greens
Vitamin C helps your body to absorb iron. Good sources of vitamin C are:
- Oranges
- Grapefruits
- Kiwi
- Strawberries
- Broccoli
- Tomatoes
Outlook (Prognosis)
With treatment, the outcome is likely to be good, but it does depend on the cause.
When to Contact a Medical Professional
Call your provider if:
- You have symptoms of iron deficiency
- You notice blood in your stool
Prevention
A balanced diet should include enough iron. Red meat, liver, and egg yolks are high sources of iron. Flour, bread, and some cereals are fortified with iron. If advised by your provider, take iron supplements if you are not getting enough iron in your diet.
Gallery
References
Brittenham GM. Disorders of iron homeostasis: iron deficiency and overload. In: Hoffman R, Benz EJ, Silberstein LE, et al, eds. Hematology: Basic Principles and Practice. 7th ed. Philadelphia, PA: Elsevier; 2018:chap 36.
Elghetany MT, Banki K. Erythrocytic disorders. In: McPherson RA, Pincus MR, eds. Henry's Clinical Diagnosis and Management by Laboratory Methods. 24th ed. Philadelphia, PA: Elsevier; 2022:chap 33.
Means RT. Approach to the anemias. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 149.
US Department of Health and Human Services; National Heart, Lung, and Blood Institute website. Iron-deficiency anemia. www.nhlbi.nih.gov/health-topics/iron-deficiency-anemia. Updated March 24, 2022. Accessed June 8, 2022.
