Primary biliary cirrhosis
Definition
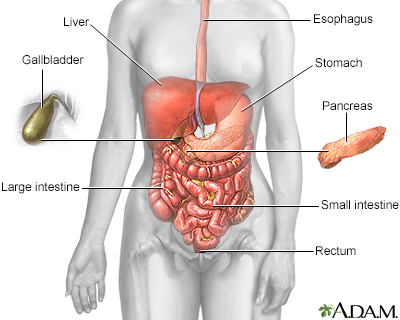
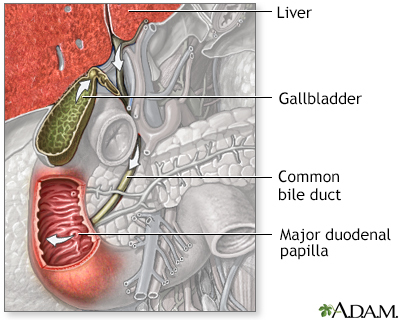
The bile ducts are tubes that move bile from the liver to the small intestine. Bile is a substance that helps with digestion. All of the bile ducts together are called the biliary tract.
When the bile ducts become swollen or inflamed, this blocks the flow of bile. These changes can lead to scarring of the liver called cirrhosis. This is called biliary cirrhosis. Advanced cirrhosis can lead to liver failure.
Alternative Names
Primary biliary cirrhosis; PBC
Causes
The cause of inflamed bile ducts in the liver is not known. However, primary biliary cholangitis is an autoimmune disorder. That means your body's immune system mistakenly attacks healthy tissue. The disease may be linked to autoimmune disorders such as:
- Celiac disease
- Raynaud phenomenon
- Sicca syndrome (dry eyes or mouth)
- Thyroid disease
The disease most often affects middle-aged women.
Symptoms
More than one half of people have no symptoms at the time of diagnosis. Symptoms most often begin slowly. Early symptoms may include:
- Nausea and belly pain
- Fatigue and loss of energy
- Fatty deposits under the skin
- Fatty stools
- Itching
- Poor appetite and weight loss
As liver function worsens, symptoms may include:
- Fluid buildup in the legs (edema) and in the abdomen (ascites)
- Yellow color in the skin, mucous membranes, or eyes (jaundice)
- Redness on the palms of the hands
- In men, impotence, shrinking of the testicles, and breast swelling
- Easy bruising and abnormal bleeding, most often from swollen veins in the digestive tract
- Confusion or problems thinking
- Pale or clay-colored stools
Exams and Tests
The health care provider will do a physical exam.
The following tests can check to see if your liver is working properly:
- Albumin blood test
- Liver function tests (serum alkaline phosphatase is most important)
- Prothrombin time (PT)
- Cholesterol and lipoprotein blood tests
Other tests that can help measure how severe liver disease may be include:
- Elevated immunoglobulin M level in the blood
- Liver biopsy
- Anti-mitochondrial antibodies (results are positive in about 95% of cases)
- Special types of ultrasound or MRI that measure the amount of scar tissue (may be called elastography)
- Magnetic resonance cholangiopancreatography (MRCP)
Treatment
The goal of treatment is to ease symptoms and prevent complications.
Cholestyramine (or colestipol) may reduce the itching. Ursodeoxycholic acid may improve removal of bile from the bloodstream. This may improve survival in some people. A newer drug called obeticholic acid (Ocaliva) is also available.
Vitamin replacement therapy restores vitamins A, K, E and D, which are lost in fatty stools. A calcium supplement or other bone medicines may be added to prevent or treat weak or soft bones.
Long-term monitoring and treatment of liver failure is needed.
Liver transplant may be successful if it is done before liver failure occurs.
Outlook (Prognosis)
The outcome can vary. If the condition is not treated, most people will die without a liver transplant. About one quarter of people who have had the disease for 10 years will have liver failure. Doctors can now use a statistical model to predict the best time to do the transplant. Other diseases, such as hypothyroidism and anemia, can also develop.
Possible Complications
Progressive cirrhosis can lead to liver failure. Complications can include:
- Bleeding
- Damage to the brain (encephalopathy)
- Fluid and electrolyte imbalance
- Kidney failure
- Malabsorption
- Malnutrition
- Soft or weak bones (osteomalacia or osteoporosis)
- Ascites (fluid buildup in the abdominal cavity)
- Increased risk of liver cancer
When to Contact a Medical Professional
Contact your provider if you have:
- Abdominal swelling
- Blood in the stools
- Confusion
- Jaundice
- Itching of the skin that does not go away and is not related to other causes
- Vomiting blood
Gallery
References
Eaton JE, Lindor KD. Primary biliary cholangitis. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 91.
Fogel EL, Sherman S. Diseases of the gallbladder and bile ducts. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 146.
Lamps LW. Liver: non-neoplastic diseases. In: Goldblum JR, Lamps LW, McKenney JK, Myers JL, eds. Rosai and Ackerman's Surgical Pathology. 11th ed. Philadelphia, PA: Elsevier; 2018:chap 19.
Smith A, Baumgartner K, Bositis C. Cirrhosis: diagnosis and management. Am Fam Physician. 2019;100(12):759-770. PMID: 31845776 pubmed.ncbi.nlm.nih.gov/31845776/.
Related specialties
Aftercare and more
Our experts
Community and Patient Programs: Primary biliary cirrhosis
Our community and patient programs provide great value to patients, families and loved ones. People can find support, educational materials, expert consultants and more. In most instances, these programs are offered free of charge.
-
Liver Support Group
This support group provides education and psychosocial support for patients who have liver disease or are awaiting liver transplants and who have been transplanted. Call (352) 265-0754 for the next scheduled meeting of the support group.
