In the right hands
At the beginning of December 2019, 16-year-old Eniyah Franklin was visiting family in Tallahassee when she decided to make herself a snack while she was alone…

Update your location to show providers, locations, and services closest to you.
A skin graft is a patch of skin that is removed by surgery from one area of the body and transplanted, or attached, to another area.
Skin transplant; Skin autografting; FTSG; STSG; Split thickness skin graft; Full thickness skin graft
This surgery is usually done while you are under general anesthesia. That means you will be asleep and pain-free.
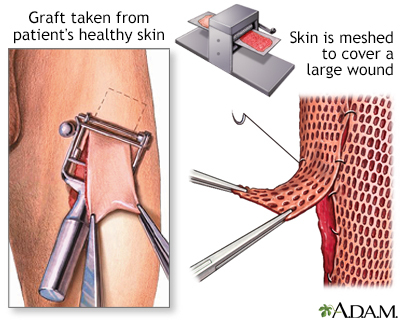
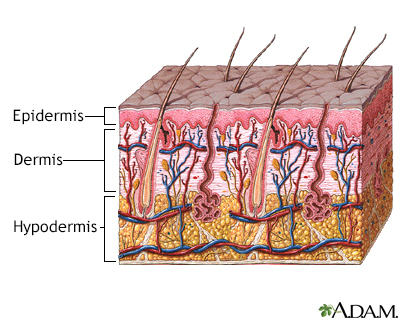
Healthy skin is taken from a place on your body called the donor site. Most people who are having a skin graft have a split-thickness skin graft. This takes the two top layers of skin from the donor site (the epidermis) and the layer under the epidermis (the dermis).
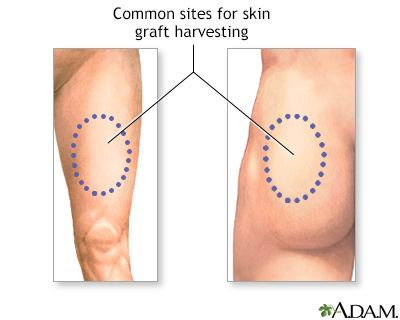
The donor site can be any area of the body. Most times, it is an area that is hidden by clothes, such as the buttock or inner thigh.
The graft is carefully spread on the bare area where it is being transplanted. It is held in place either by gentle pressure from a well-padded dressing that covers it, or by staples or a few small stitches. The donor-site area is covered with a sterile dressing for 3 to 5 days.
People with deeper tissue loss may need a full-thickness skin graft. This requires the entire thickness of skin from the donor site, not just the top two layers.
A full-thickness skin graft is a more complicated procedure. Common donor sites for full-thickness skin grafts include the chest wall, neck, back, or abdominal wall.
Skin grafts may be recommended for:
Full-thickness grafts are done when a lot of tissue is lost. This can happen with open fractures of the lower leg, or after severe infections.
Risks for anesthesia and surgery in general are:
Risks for this surgery are:
Tell your surgeon or nurse:
During the days before surgery:
On the day of the surgery:
You should recover quickly after split-thickness skin grafting. Full-thickness grafts need a longer recovery time. If you received this kind of graft, you may need to stay in the hospital for recovery.
After you are discharged from the hospital, follow instructions on how to care for your skin graft, including:
Most skin grafts are successful, but some do not heal well. You may need a second graft.
Padilla PL, Khoo KH, Ho T, Cole EL, Sirvent RZ, Phillips LG. Plastic surgery. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 69.
Ratner D, Nayyar PM. Grafts, In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018:chap 148.
Scherer-Pietramaggiori SS, Pietramaggiori G, Orgill DP. Skin graft. In: Gurtner GC, Neligan PC, eds. Plastic Surgery, Volume 1: Principles. 4th ed. Philadelphia, PA: Elsevier; 2018:chap 15.


Our community and patient programs provide great value to patients, families and loved ones. People can find support, educational materials, expert consultants and more. In most instances, these programs are offered free of charge.
Offers a wide variety of music-based therapies from in-room performances to collaborative recording sessions.
At the beginning of December 2019, 16-year-old Eniyah Franklin was visiting family in Tallahassee when she decided to make herself a snack while she was alone…

All 13-year-old Gabby Carrara wanted to do on a June afternoon in 2013 was exercise her newly acquired teen freedom. It was a Sunday, and her parents had…
