Definition
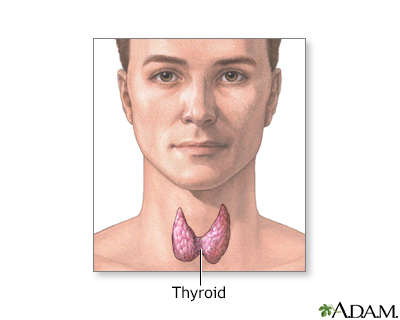
Medullary carcinoma of the thyroid is cancer of the thyroid gland that starts in cells that release a hormone called calcitonin. These cells are called "C" cells. The thyroid gland is located inside the front of your lower neck.
Alternative Names
Thyroid - medullary carcinoma; Cancer - thyroid (medullary carcinoma); MTC; Thyroid nodule - medullary
Causes
The cause of medullary carcinoma of the thyroid (MTC) is unknown. MTC is very rare. It can occur in children and adults.
Unlike other types of thyroid cancer, MTC is less likely to be caused by radiation therapy to the neck given to treat other cancers during childhood.
There are two forms of MTC:
-
Sporadic MTC, which does not run in families. Most MTCs are sporadic. This form mainly affects older adults.
- Hereditary MTC, which runs in families.
You have an increased risk for this type of cancer if you have:
Other types of thyroid cancer include:
Symptoms
MTC often begins as a small lump (nodule) in the thyroid gland. There also may be lymph node swelling in the neck. As a result, symptoms may include:
- Swelling of the neck
- Hoarseness
- Breathing problems due to narrowing of airways
- Cough
- Cough with blood
- Diarrhea due to high calcitonin level
Exams and Tests
Your health care provider will perform a physical exam and ask about your symptoms and medical history.
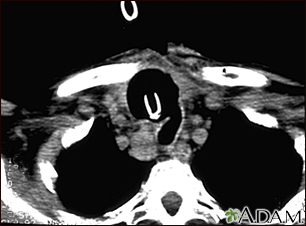
Tests that may be used to diagnose MTC include:
People with MTC should be checked for certain other tumors, especially pheochromocytoma and parathyroid tumors and parathyroid tumors.
Treatment
Treatment involves surgery to remove the thyroid gland and surrounding lymph nodes. Because this is an uncommon tumor, surgery should be performed by a surgeon who is familiar with this type of cancer and experienced with the operation required.
Further treatment will depend on your calcitonin levels. A rise in calcitonin levels again may indicate new growth of the cancer.
- Chemotherapy and radiation do not work very well for this type of cancer.
- Radiation is used in some people after surgery.
- Newer targeted therapies may reduce tumor growth also. Your provider can tell you more about these, if needed.
Near relatives of persons diagnosed with hereditary forms of MTC are at increased risk of this cancer and should discuss with their providers.
Support Groups
You can ease the stress of illness by joining a cancer support group. Sharing with others who have common experiences and problems can help you not feel alone.
Outlook (Prognosis)
Most people with MTC live at least 5 years after diagnosis, depending upon the stage of the cancer. The 10-year survival rate is 65%.
Possible Complications
Complications may include:
-
Cancer spreads to other areas of the body
-
Parathyroid glands are accidentally removed during surgery
When to Contact a Medical Professional
Contact your provider if you have symptoms of MTC.
Prevention
Prevention may not be possible. But, being aware of your risk factors, especially your family history, may allow for early diagnosis and treatment. For people who have a very strong family history of MTC, the option to remove the thyroid gland may be recommended. You should carefully discuss this option with a doctor who is very familiar with the disease.
References
Insoo S, Sosa JA. Thyroid. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. Philadelphia, PA: Elsevier; 2022:chap 37.
Jonklass J, Cooper DS. Thyroid. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 213.
National Cancer Institute website. Thyroid cancer treatment (adult) (PDQ) - health professional version. www.cancer.gov/types/thyroid/hp/thyroid-treatment-pdq. Updated February 18, 2022. Accessed June 14, 2022.
Viola D, Elisei R. Management of medullary thyroid cancer. Endocrinol Metab Clin North Am. 2019;48(1):285-301. PMID: 30717909 pubmed.ncbi.nlm.nih.gov/30717909/.
Wells SA Jr, Asa SL, Dralle H. Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid. 2015;25(6):567-610. PMID: 25810047 pubmed.ncbi.nlm.nih.gov/25810047/.