Diabetes - taking care of your feet
Description
Diabetes can damage the nerves and blood vessels in your feet. This damage can cause numbness and reduce feeling in your feet. As a result, your feet are more likely to become injured and may not heal well if they are injured. If you get a blister, you may not notice and it may get worse. Even small sores or blisters can become big problems if infection develops or they don't heal. A diabetic foot ulcer can result. Foot ulcers are a common reason for hospital stays for people with diabetes. Taking good care of your feet can help prevent diabetic foot ulcers. Untreated foot ulcers are the most common reason for toe, foot, and leg amputations in people with diabetes.
Patient Education Video: Diabetes
Alternative Names
Diabetes - foot care - self-care; Diabetic foot ulcer - foot care; Diabetic neuropathy - foot care
Self-care
Follow your health care provider's instructions on how to take care of your feet. Use the information below as a reminder.
Check your feet every day. Inspect the tops, sides, soles, heels, and between your toes. Look for:
- Dry and cracked skin
- Blisters or sores
- Bruises or cuts
- Redness, warmth, or tenderness (often absent because of nerve damage)
- Firm or hard spots
If you cannot see well, ask someone else to check your feet.
Wash your feet every day with lukewarm water and mild soap. Strong soaps may damage the skin.
- Check the temperature of the water with your hand or elbow first.
- Gently dry your feet, especially between the toes.
- Use lotion, petroleum jelly, lanolin, or oil on dry skin. Do not put lotion, oil, or cream between your toes.
Ask your provider to show you how to trim your toenails.
- Soak your feet in lukewarm water to soften your toenails before trimming.
- Cut the nails straight across. Curved nails are more likely to become ingrown.
- Make sure the edge of each nail does not press into the skin of the next toe.
Do not try to cut very thick toenails by yourself. Your foot doctor (podiatrist) can trim your toenails if you are unable to. If your toenails are thick and discolored (possibly due to a fungal infection) do not trim the nails yourself. If your vision is poor or you have decreased sensation in your feet, you should see a podiatrist to trim your toenails to prevent possible injury.
Most people with diabetes should have corns or calluses treated by a foot doctor. If your doctor has given you permission to treat corns or calluses on your own:
- Gently use a pumice stone to remove corns and calluses after a shower or bath, when your skin is soft.
- Don't use medicated pads or try to shave or cut corns and calluses away at home.
If you smoke, stop. Smoking decreases blood flow to your feet. Talk to your provider or nurse if you need help quitting.
Do not use a heating pad or hot water bottle on your feet. Don't walk barefoot, particularly on hot pavement, hot tiles, or hot, sandy beaches. This can cause severe burns in people with diabetes because the skin does not respond normally to the heat.
Remove your shoes and socks during visits to your provider so that they can check your feet.
Shoes and Socks
Wear shoes at all times to protect your feet from injury. Before you put them on, always check the inside of your shoes for stones, nails, or rough areas that may hurt your feet.
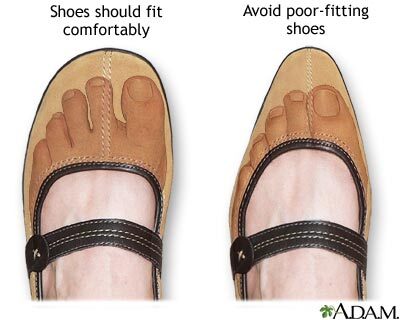
Wear shoes that are comfortable and fit well when you buy them. Never buy shoes that are tight, not even if you think they will stretch as you wear them. You may not feel pressure from shoes that do not fit well. Blisters and sores can develop when your foot presses against your shoe.
Ask your provider about special shoes that can give your feet more room. When you get new shoes, break them in slowly. Wear them 1 or 2 hours a day for the first 1 or 2 weeks.
Change your broken-in shoes after 5 hours during the day to change the pressure points on your feet. Do not wear flip-flop sandals or stockings with seams. Both can cause pressure points.
To protect your feet, wear clean, dry socks or non-binding panty hose every day. Holes in socks or stockings can put damaging pressure on your toes.
You may want special socks with extra padding. Socks that move moisture away from your feet will keep your feet drier. In cold weather, wear warm socks, and do not stay out in the cold for very long. Wear clean, dry socks to bed if your feet are cold.
When to Call the Doctor
Call your provider right way about any foot problems you have. Do not try to treat these problems yourself. Call your provider if you have any of the following changes to any part of your foot:
- Redness, increased warmth, or swelling
- Sores or cracks
- Tingling or burning feeling
- Pain
Gallery


References
American Diabetes Association. 12. Retinopathy, neuropathy, and foot care-2022. Diabetes Care. 2022;45(Suppl 1):S185-S194. PMID: 34964887 pubmed.ncbi.nlm.nih.gov/34964887/.
Brownlee M, Aiello LP, Sun JK, et al. Complications of diabetes mellitus. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 37.
Centers for Disease Control and Prevention website. Diabetes and your feet. www.cdc.gov/diabetes/library/features/healthy-feet.html. Updated June 20, 2022. Accessed August 26, 2022.