Hypotonia
Definition
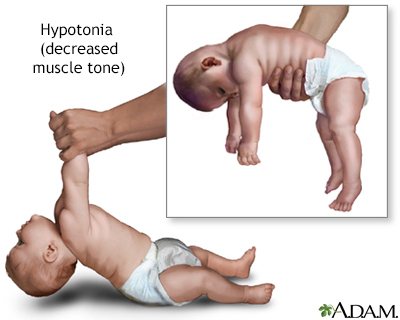
Hypotonia means decreased muscle tone.
Alternative Names
Decreased muscle tone; Floppy infant
Considerations
Hypotonia is often a sign of a worrisome problem. The condition can affect children or adults.
Infants with this problem seem floppy and feel like a "rag doll" when held. They rest with their elbows and knees loosely extended. Infants with normal tone tend to have flexed elbows and knees. They may have poor head control. The head may fall to the side, backward, or forward.
Infants with normal tone can be lifted with the adult's hands placed under the armpits. Hypotonic infants tend to slip between the hands.
Causes
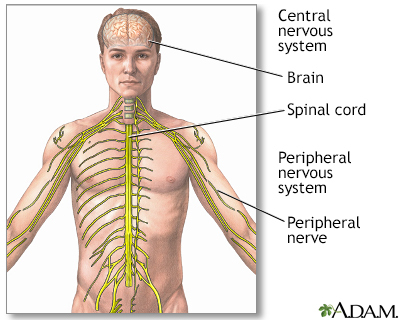
Muscle tone and movement involve the brain, spinal cord, nerves, and muscles. Hypotonia may be a sign of a problem anywhere along the pathway that controls muscle movement. Causes may include:
- Brain damage, due to lack of oxygen before or right after birth, or problems with brain formation
- Disorders of the muscles, such as muscular dystrophy
- Disorders that affect the nerves that supply muscles
- Disorders that affect the ability of nerves to send messages to the muscles
- Infections
Genetic or chromosomal disorders, or defects that may cause brain and nerve damage include:
Other disorders that can lead to the condition include:
- Achondroplasia
- Being born with hypothyroidism
- Poisons or toxins
- Spinal cord injuries that occur around the time of birth
Home Care
Take extra care when lifting and carrying a person with hypotonia to avoid causing an injury.
What to Expect at Your Office Visit
The physical exam will include a detailed examination of the nervous system and muscle function.
In most cases, a neurologist (specialist in brain and nerve disorders) will help evaluate the problem. Geneticists may help diagnose certain disorders. If there are also other medical problems, a number of different specialists will help care for the child.
Which diagnostic tests are done depends on the suspected cause of the hypotonia. Most of the conditions associated with hypotonia also cause other symptoms that can help in the diagnosis.
Many of these disorders require ongoing care and support. Physical therapy may be recommended to help children improve their development.
Gallery
References
Burnette WB. Hypotonic (floppy) infant. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 30.
Johnston MV. Encephalopathies. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 616.
Marcdante KJ, Kliegman RM, Schuch AM. Weakness and hypotonia. In: Marcdante KJ, Kliegman RM, Schuch AM, eds. Nelson Essentials of Pediatrics. 9th ed. Elsevier; 2023:chap 182.
Sarnat HB. Evaluation and investigation of neuromuscular disorders. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 625.