Skin findings in newborns
Definition
A newborn infant's skin goes through many changes both in appearance and texture.
Alternative Names
Newborn skin characteristics; Infant skin characteristics; Neonatal care - skin
Information
The skin of a healthy newborn at birth has:
- Deep red or purple skin and bluish hands and feet. The skin darkens before the infant takes their first breath (when they make that first vigorous cry).
- A thick, waxy substance called vernix covering the skin. This substance protects the fetus's skin from the amniotic fluid in the womb. Vernix should wash off during the baby's first bath.
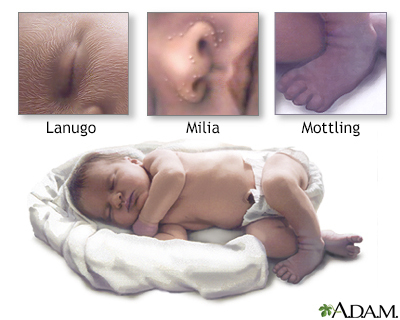
- Fine, soft hair (lanugo) that may cover the scalp, forehead, cheeks, shoulders, and back. This is more common when an infant is born before the due date. The hair should disappear within the first few weeks of the baby's life.
Newborn skin will vary, depending on the length of the pregnancy. Premature infants have thin, transparent skin. The skin of a full-term infant is thicker.
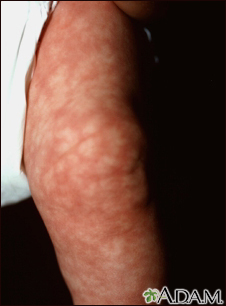
By the baby's second or third day, the skin lightens somewhat and may become dry and flaky. The skin still often turns red when the infant cries. The lips, hands, and feet may turn bluish or spotted (mottled) when the baby is cold.
Other changes may include:
- Milia, (tiny, pearly-white, firm raised bumps on the face) which disappear on their own.
- Mild acne that most often clears in a few weeks. This is caused by some of the mother's hormones that stay in the baby's blood.
- Erythema toxicum. This is a common, harmless rash that looks like little pustules on a red base. It tends to appear on the face, trunk, legs, and arms about 1 to 3 days after delivery. It disappears by 1 week.
Colored birthmarks or skin markings may include:
- Congenital nevi are moles (darkly pigmented skin markings) that may be present at birth. They range in size from as small as a pea to large enough to cover an entire arm or leg, or a large portion of the back or trunk. Larger nevi carry a greater risk of becoming skin cancer. The health care provider should follow all nevi.
- Mongolian spots are blue-gray or brown spots. They can emerge on the skin of the buttocks or back, mainly in dark-skinned babies. They should fade within a year.
- Café-au-lait spots are light tan, the color of coffee with milk. They often appear at birth, or may develop within the first few years. Children who have many of these spots, or large spots, may be more likely to have a condition called neurofibromatosis.
Red birthmarks may include:
- Port-wine stains -- growths that contain blood vessels (vascular growths). They are red to purplish in color. They are frequently seen on the face, but may occur on any area of the body.
- Hemangiomas -- a collection of capillaries (small blood vessels) that may appear at birth or a few months later.
- Stork bites -- small red patches on the baby's forehead, eyelids, back of the neck, or upper lip. They are caused by stretching of the blood vessels. They often go away within 18 months.
Gallery





References
Balest AL, Riley MM, O'Donnell B, Zarit JS . Neonatology. In: Zitelli BJ, McIntire SC, Nowalk AJ, Garrison J, eds. Zitelli and Davis' Atlas of Pediatric Physical Diagnosis. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 2.
Bender NR, Chiu YE. Dermatological evaluation of the patient. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 664.
Narendran V. The skin of the neonate. In: Martin RJ, Fanaroff AA, Walsh MC, eds. Fanaroff and Martin's Neonatal-Perinatal Medicine. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 94.
Walker VP. Newborn evaluation. In: Gleason CA, Juul SE, eds. Avery's Diseases of the Newborn. 10th ed. Philadelphia, PA: Elsevier; 2018:chap 25.