Tay-Sachs disease
Definition
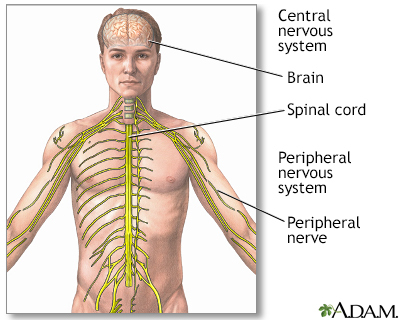
Tay-Sachs disease is a life-threatening disease of the nervous system passed down through families.
Alternative Names
GM2 gangliosidosis - Tay-Sachs; Lysosomal storage disease - Tay-Sachs disease
Causes
Tay-Sachs disease occurs when the body lacks hexosaminidase A. This is a protein that helps break down a group of chemicals found in nerve tissue called gangliosides. Without this protein, gangliosides, particularly ganglioside GM2, build up in cells, often nerve cells in the brain.
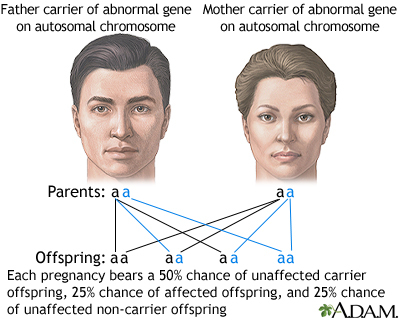
Tay-Sachs disease is caused by a defective gene on chromosome 15. When both parents carry the defective Tay-Sachs gene, a child has a 25% chance of developing the disease. The child must receive two copies of the defective gene, one from each parent, in order to become sick. If only one parent passes the defective gene to the child, the child is called a carrier. They will not be sick, but may pass the disease to their own children.
Anyone can be a carrier of the Tay-Sachs gene. But, the disease is most common among people with Ashkenazi Jewish ancestry, where 1 in every 27 people carries the Tay-Sachs gene.
Tay-Sachs is divided into infantile, juvenile, and adult forms, depending on the symptoms and when they first appear. Most people with Tay-Sachs have the infantile form. In this form, the nerve damage usually begins while the baby is still in the womb. Symptoms usually appear when the child is 3 to 6 months old. The disease tends to get worse very quickly, and the child usually dies by age 4 or 5.
Late-onset Tay-Sachs disease, which affects adults, is very rare.
Symptoms
Symptoms may include any of the following:
- Deafness
- Decreased eye contact, blindness
- Decreased muscle tone (loss of muscle strength), loss of motor skills, paralysis
- Slow growth and delayed mental and social skills
- Dementia (loss of brain function)
- Increased startle reaction
- Irritability
- Listlessness
- Seizures
Exams and Tests
The health care provider will examine your baby and ask about your family history. Tests that may be done are:
Treatment
There is no treatment for Tay-Sachs disease itself, only ways to make the person more comfortable.
Support Groups
The stress of illness may be eased by joining support groups whose members share common experiences and problems. The following groups can provide more information on Tay-Sachs disease:
- National Organization for Rare Disorders -- rarediseases.org/rare-diseases/tay-sachs-disease
- National Tay-Sachs and Allied Diseases Association -- www.ntsad.org
- NLM Genetics Home Reference -- ghr.nlm.nih.gov/condition/tay-sachs-disease
Outlook (Prognosis)
Children with this disease have symptoms that get worse over time. They usually die by age 4 or 5.
Possible Complications
Symptoms appear during the first 3 to 10 months of life and progress to spasticity, seizures, and loss of all voluntary movements.
When to Contact a Medical Professional
Go to the emergency room or call 911 or the local emergency number if:
- Your child has a seizure of unknown cause
- The seizure is different from previous seizures
- The child has difficulty breathing
- The seizure lasts longer than 2 to 3 minutes
Contact your provider for an appointment if your child has other noticeable behavioral changes.
Prevention
There is no known way to prevent this disorder once someone is born. Genetic testing can detect if you are a carrier of the gene for this disorder. If you or your partner is from an at-risk population, you may wish to seek genetic counseling before starting a family.
If you are already pregnant, testing the amniotic fluid can diagnose Tay-Sachs disease in the womb.
Gallery
References
Kwon JM. Neurodegenerative disorders of childhood. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 617.
Nussbaum RL, McInnes RR, Willard HF. The molecular, biochemical, and cellular basis of genetic disease. In: Nussbaum RL, McInnes RR, Willard HF, eds. Thompson & Thompson Genetics in Medicine. 8th ed. Philadelphia, PA: Elsevier; 2016:chap 12.
Wapner RJ, Dugoff L. Prenatal diagnosis of congenital disorders. In: Resnik R, Lockwood CJ, Moore TR, Greene MF, Copel JA, Silver RM, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 32.