Trench mouth
Definition
Trench mouth is an infection that causes swelling (inflammation) and ulcers in the gums (gingivae). The term trench mouth comes from World War I, when this infection was common among soldiers "in the trenches."
Alternative Names
Vincent's stomatitis; Acute necrotizing ulcerative gingivitis (ANUG); Vincent disease
Causes
Trench mouth is a painful form of gum swelling (gingivitis). The mouth normally contains a balance of different bacteria. Trench mouth occurs when there is too much pathologic bacteria. The gums become infected and develop painful ulcers. Viruses may be involved in allowing the bacteria to grow too much.
Things that increase your risk of trench mouth include:
- Emotional stress (such as studying for exams)
- Poor oral hygiene
- Poor nutrition
- Smoking
- Weak immune system
- Throat, tooth, or mouth infections
Trench mouth is rare. When it does occur, it most often affects people ages 15 to 35.
Symptoms
Symptoms of trench mouth often begin suddenly. They include:
- Bad breath
- Crater-like ulcers between the teeth
- Fever
- Foul taste in the mouth
- Gums appear red and swollen
- Grayish film on the gums
- Painful gums
- Severe gum bleeding in response to any pressure or irritation
Exams and Tests
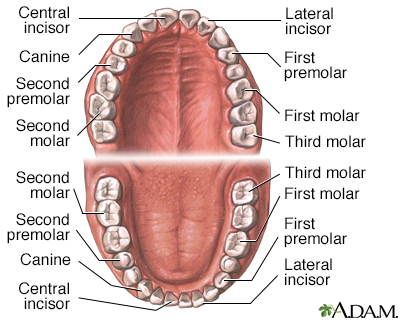
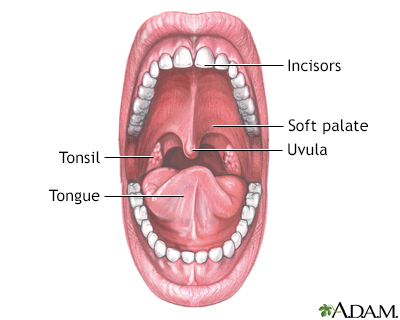
The health care provider will look into your mouth for signs of trench mouth, including:
- Crater-like ulcers filled with plaque and food debris
- Destruction of gum tissue around the teeth
- Inflamed gums
There may be a gray film caused by broken down gum tissue. In some cases, there may be fever and swollen lymph nodes of the head and neck.
Dental x-rays or x-rays of the face may be taken to determine how severe the infection is and how much tissue has been destroyed.
This disease may also be tested for by using a throat swab culture.
Treatment
The goals of treatment are to cure the infection and relieve symptoms. Your provider may prescribe antibiotics if you have a fever.
Good oral hygiene is vital to the treatment of trench mouth. Brush and floss your teeth thoroughly at least twice a day, or after each meal and at bedtime, if possible.
Salt-water rinses (one half teaspoon or 3 grams of salt in 1 cup or 240 milliliters of water) may soothe sore gums. Hydrogen peroxide, used to rinse the gums, is often recommended to remove dead or dying gum tissue. Chlorhexidine rinse will help with gum inflammation.
Over-the-counter pain relievers may reduce your discomfort. Soothing rinses or coating agents may reduce pain, especially before eating. You may apply lidocaine to your gums for severe pain.
You may be asked to visit a dentist or dental hygienist to have your teeth professionally cleaned and to have the plaque removed, once your gums feel less tender. You may need to get numb for the cleaning. You may need frequent dental cleaning and examinations until the disorder is cleared.
To prevent the condition from coming back, your provider may give you instructions on how to:
- Maintain good general health, including proper nutrition and exercise
- Maintain good oral hygiene
- Reduce stress
- Stop smoking
Avoid irritants such as smoking and hot or spicy foods.
Outlook (Prognosis)
The infection usually responds to treatment. The disorder can be quite painful until it is treated. If trench mouth is not treated promptly, the infection can spread to the cheeks, lips, or jawbone. It can destroy these tissues.
Possible Complications
Complications of trench mouth include:
- Dehydration
- Weight loss
- Loss of teeth
- Pain
- Gum infection (periodontitis)
- Spread of infection
When to Contact a Medical Professional
Contact a dentist if you have symptoms of trench mouth, or if fever or other new symptoms develop.
Prevention
Preventive measures include:
- Good general health
- Good nutrition
- Good oral hygiene, including thorough tooth brushing and flossing
- Learning ways to cope with stress
- Regular professional dental cleaning and exams
- Stopping smoking
Gallery
References
Chow AW. Infections of the oral cavity, neck, and head. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 64.
Simon L, Silk H. Diseases of the mouth. In: Kellerman RD, Rakel DP, eds. Conn's Current Therapy 2022. Philadelphia, PA: Elsevier; 2022:1048-1053.
James WD, Elston DM, Treat JR, Rosenbach MA, Neuhaus IM. Disorders of the mucous membranes. In: James WD, Elston DM, Treat JR, Rosenbach MA, Neuhaus IM, eds. Andrews' Diseases of the Skin: Clinical Dermatology. 13th ed. Philadelphia, PA: Elsevier; 2020:chap 34.