Wilson disease
Definition
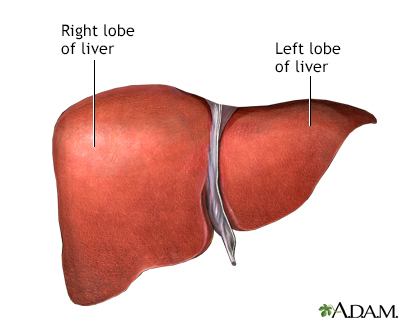
Wilson disease is an inherited disorder in which there is too much copper in the body's tissues. The excess copper damages the liver and nervous system.
Alternative Names
Wilson's disease; Hepatolenticular degeneration
Causes
Wilson disease is a rare inherited disorder. If both parents carry a defective gene for Wilson disease, there is a 25% chance in each pregnancy that the child will have the disorder.
Wilson disease causes the body to take in and keep too much copper. The copper deposits in the liver, brain, kidneys, and eyes. This causes tissue damage, tissue death, and scarring. The affected organs stop working normally.
This condition is most common in eastern Europeans, Sicilians, and southern Italians, but it may occur in any group. Wilson disease symptoms typically appears in people under 40 years old. In children, the symptoms begin to show by age 4.
Symptoms
Symptoms may include:
- Abnormal posture of arms and legs
- Arthritis
- Confusion or delirium
- Dementia
- Difficulty moving arms and legs, stiffness
- Difficulty walking (ataxia)
- Emotional or behavioral changes
- Enlargement of the abdomen due to accumulation of fluid (ascites)
- Personality changes
- Phobias
- Slow movements
- Slow or decreased movement and expressions of the face
- Speech impairment
- Tremors of the arms or hands
- Uncontrollable movement
- Unpredictable and jerky movement
- Vomiting blood
- Weakness
- Yellow skin (jaundice) or yellow color of the white of the eye (icterus)
Exams and Tests
A slit-lamp eye exam may show:
- Limited eye movement
- Rusty or brown-colored ring around the iris (Kayser-Fleischer rings)
A physical exam may show signs of:
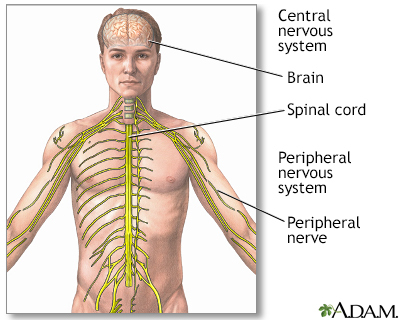
- Damage to the central nervous system, including loss of coordination, loss of muscle control, muscle tremors, loss of thinking and IQ, loss of memory, and confusion (delirium or dementia)
- Liver or spleen disorders (including hepatomegaly and splenomegaly)
Lab tests may include:
- Complete blood count (CBC)
- Serum ceruloplasmin
- Serum copper
- Serum uric acid
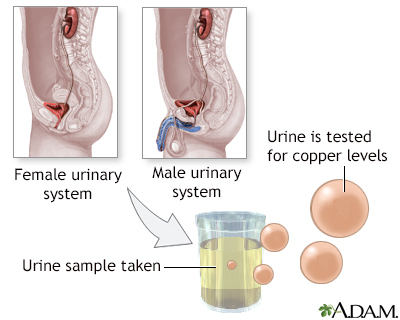
- Urine copper
If there are liver problems, lab tests may find:
Other tests may include:
- 24-hour urine copper test
- Abdominal x-ray
- Abdominal MRI
- CT scan of the abdomen
- Head CT scan
- Head MRI
- Liver biopsy
- Upper GI endoscopy
The gene that causes Wilson disease has been found. It is called ATP7B. DNA testing is available for this gene. Talk to your health care provider or a genetic counselor to learn if you should have gene testing performed.
Treatment
The goal of treatment is to reduce the amount of copper in the tissues. This is done by a procedure called chelation. Certain medicines are given that bind to copper and help remove it through the kidneys or gut. Treatment must be lifelong.
The following medicines may be used:
- Penicillamine (such as Cuprimine, Depen) binds to copper and leads to increased release of copper in the urine.
- Trientine (such as Syprine) binds (chelates) the copper and increases its release through the urine.
- Zinc acetate (such as Galzin) blocks copper from being absorbed in the intestinal tract.
Vitamin E supplements may also be used.
Sometimes, medicines that chelate copper (such as penicillamine) can affect the function of the brain and nervous system (neurological function). Other medicines under investigation may bind copper without affecting neurological function.
A low-copper diet may also be recommended. Foods to avoid include:
- Chocolate
- Dried fruit
- Liver
- Mushrooms
- Nuts
- Shellfish
You may want to drink distilled water because some tap water flows through copper pipes. Avoid using copper cooking utensils.
Symptoms may be managed with exercise or physical therapy. People who are confused or unable to care for themselves may need special protective measures.
A liver transplant may be considered in cases where the liver is severely damaged by the disease.
Support Groups
More information and support for people with Wilson disease and their families can be found at:
- Wilson Disease Association: - wilsondisease.org
- Genetic Alliance: - geneticalliance.org
Outlook (Prognosis)
Lifelong treatment is needed to control Wilson disease. The disorder may cause fatal effects, such as loss of liver function. Copper can have toxic effects on the nervous system. In cases where the disorder is not fatal, symptoms may be disabling.
Possible Complications
Complications may include:
- Anemia (hemolytic anemia is rare)
- Central nervous system complications
- Cirrhosis
- Death of liver tissues
- Fatty liver
- Hepatitis
- Increased chances of bone fractures
- Increased number of infections
- Injury caused by falls
- Jaundice
- Joint contractures or other deformity
- Loss of ability to care for self
- Loss of ability to function at work and home
- Loss of ability to interact with other people
- Loss of muscle mass (muscle atrophy)
- Psychological complications
- Side effects of penicillamine and other medicines used to treat the disorder
- Spleen problems
Liver failure and damage to the central nervous system (brain, spinal cord) are the most common and dangerous effects of the disorder. If the disease is not caught and treated early, it can be fatal.
When to Contact a Medical Professional
Contact your provider if you have symptoms of Wilson disease. Contact a genetic counselor if you have a history of Wilson disease in your family and you are planning to have children.
Prevention
Genetic counseling is recommended for people with a family history of Wilson disease.
Gallery
References
National Institute of Diabetes and Digestive and Kidney Diseases website. Wilson disease. www.niddk.nih.gov/health-information/liver-disease/wilson-disease/definition-facts. Updated October 2018. Accessed November 11, 2022.
Roberts EA. Wilson disease. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 76.
Schilsky ML. Wilson disease. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 200.