UF Health study: Specific immunotherapy allows for safer, more effective gene therapy
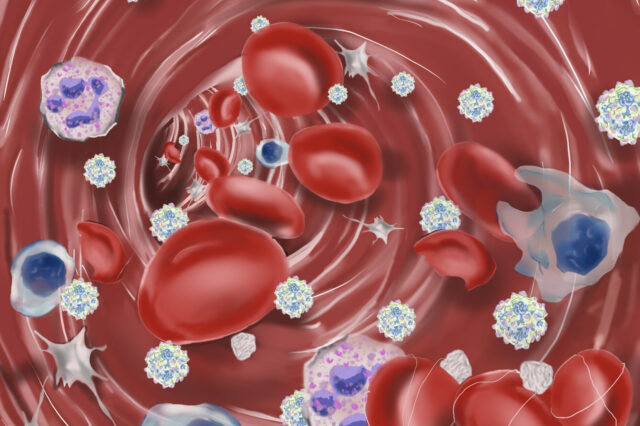
Red blood cells, lymphocytes, neutrophils, macrophages, and platelets are pictured flowing through the blood stream alongside adeno associated viral (AAV) particles. The AAV particles trigger the innate immune system as illustrated by activated platelets, blood clot formation and fragmented red blood cells (schistocytes) in the foreground. (Image courtesy of Stephanie Salabarria/UF Health)
Gene therapy could become safer and more effective by calming the inflammation that occurs when the treatment is administered, University of Florida Health researchers have found.
The therapy uses a harmless, engineered virus to deliver a functioning copy of a defective gene. Unfortunately for patients, the body often reacts to the gene therapy by launching an immune-system response that can be problematic.
Now, researchers say they have found a solution that quells life-threatening immune system responses during adeno-associated virus gene therapy, or AAV. The inflammation arising from AAV treatments can cause kidney injury, liver toxicity and a condition known as thrombotic microangiopathy, which destroys red blood cells and damages organs with microscopic blood clots.
The findings should improve safety by blocking antibody responses before gene therapy is administered, said Barry J. Byrne, M.D., Ph.D., a co-author of the study, a professor and associate chair for research in the UF College of Medicine’s department of pediatrics and the Earl and Christy Powell university chair in genetics. Antibodies are bloodborne proteins that recognize and neutralize foreign substances. The findings were published Tuesday in the Journal of Clinical Investigation.
Blocking a torrent of antibodies can have a doubly beneficial effect.
“Not only can it enhance safety, we believe it also increases the effectiveness of the gene therapy treatment when antibodies are prevented,” Byrne said.
In their study, the researchers assessed 38 patients of all ages who had received an AAV9 treatment for various neuromuscular disorders. A conventional steroid treatment to prevent antibodies was given to 23 of the study participants. Another group of 15 patients received steroids along with rituximab and sirolimus, which are immune system suppressors. The patients who received only the steroid had rapid increases in two types of antibodies. The children treated with steroids and the two immunosuppressants showed no major change in antibody levels.
Steroids have long been a mixed bag for AAV patients, quelling the inflammation in cells that occurs during a gene therapy treatment but doing nothing to block the antibody response. Gene therapy patients often require increasingly larger doses of steroids for longer periods of time, raising the risk of side effects. The findings by Byrne and his collaborators potentially change all that.
“We found that we can reduce and almost eliminate steroid use with this more specific, targeted therapy,” Byrne said.
The finding that the two-drug combination of rituximab and sirolimus can prevent abnormal responses to AAV therapy is particularly encouraging, said Manuela Corti, Ph.D., a co-author of the paper and associate director of UF College of Medicine’s Powell Gene Therapy Center. The paper is one of the first to characterize what happens with the immune response after a gene therapy is administered, she said.
The discovery also represents a potential breakthrough for the thousands of patients in the U.S. who receive gene therapy each year. About one-half of adults and almost one-third of children are ineligible for gene therapy due to antibody issues. Pretreating more patients with the two-drug combination could help address that issue, Byrne said.
Next, the researchers plan to use machine learning, a form of artificial intelligence, to compare the genetic information of people who had adverse reactions to gene therapy with those who did not.
“We hope we can identify risk factors based on the genetic profile of the patient being treated. The idea is to identify the people who might need more aggressive management of potential adverse events before they occur,” Byrne said.
Scientists from the National Institutes of Health, Indiana University, 4D Molecular Therapeutics and Rocket Pharmaceuticals collaborated on the research.
About the author
