UF researchers’ genetic detection discovery has implications for medical diagnostic testing
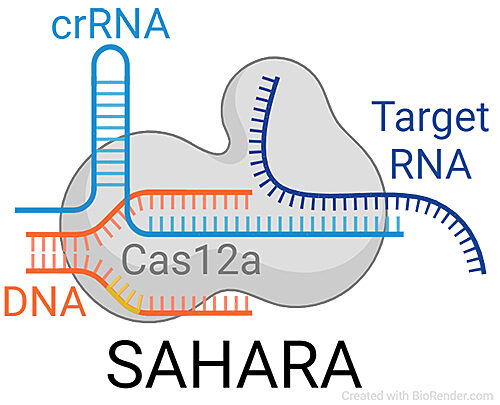
An illustration of how the CRISPR-Cas12a protein complex detects RNA. The method, developed in the lab of Piyush Jain, Ph.D., is known as Split Activator for Highly Accessible RNA analysis, or SAHARA.
University of Florida researchers have found a new use for “genetic scissors” to detect RNA, a discovery that could lead to faster, more accurate and less expensive diagnostic tests for a host of diseases.
The genetic scissors are a protein complex known as CRISPR-Cas12a. Until now, it had only been known to bind and cleave DNA, a molecule that holds life-giving genetic codes. Knowing that the genetic scissors can also bind RNA — the genetic cousin to DNA — gives scientists a crucial shortcut for designing future medical diagnostic tests.
By directly targeting RNA, tests for hepatitis, HIV, cancer and other disorders also might become simpler and less prone to false positives, said Piyush K. Jain, Ph.D., the study’s lead investigator, a Shah Rising Star assistant professor of chemical engineering and an affiliate assistant professor of molecular genetics in the UF College of Medicine. The group’s findings were published recently in the journal Nature Communications.
Testing for RNA viruses is currently a multi-step process: First, RNA must be converted into DNA. Then, many additional copies of the complementary DNA need to be generated before the virus can be detected. This takes time and can lead to lost genetic information and more false-positive tests. Cutting and detecting RNA directly with CRISPR-Cas12a can make many of those time-consuming and problematic issues go away, Jain said.
While developing robust, clinical diagnostic tests will require more work, Jain said the technique has the potential to improve the speed and accuracy of testing for viruses like the one that causes COVID-19. Directly detecting viral RNA could lead to an in-home COVID-19 test that combines the affordability, speed and convenience of a rapid antigen test with the reliability and accuracy of another type of test that still requires laboratory work.
“We want to break through that big barrier of multiple testing that is required. The idea is to bring the precision testing into homes, doctors’ offices and even airports,” Jain said.
The U.S. Food and Drug Administration has already granted Emergency Use Authorization for multiple other CRISPR-based COVID-19 tests developed elsewhere but Jain said they need to be conducted in a lab and can be costly and time-consuming.
“What we want to do is develop a test that is simple but also accurate and less expensive,” said Jain, who is also a member of the UF Health Cancer Center.
To establish their findings, the researchers developed a tool for direct RNA detection using Cas12a. It was validated with testing on RNA from hepatitis C, which is a viral infection of the liver, and a molecule known as miRNA-155 that drives breast cancer progression. The detection tool was able to “robustly detect” the target RNA in both cases, the researchers found.
More broadly, Jain said the CRISPR-Cas12a technique might also be used to detect diseases arising from genetic mutations, such as the inherited blood disorders beta thalassemia and sickle cell anemia, and various types of cancers.
For Jain, the technique holds promise for simplifying diagnostic testing and quickly identifying a wide range of diseases.
“The beauty of this approach is its exceptional versatility,” Jain said. “You can change your target and detect a lot of different things.”
Next, the technology needs to be licensed to a business that can further develop it and acquire FDA approval, Jain said. Research funding was provided by UF and its Herbert Wertheim College of Engineering, the Florida Breast Cancer Foundation and the National Institutes of Health.
About the author
