New tool for assessing dehydration is built for global deployment
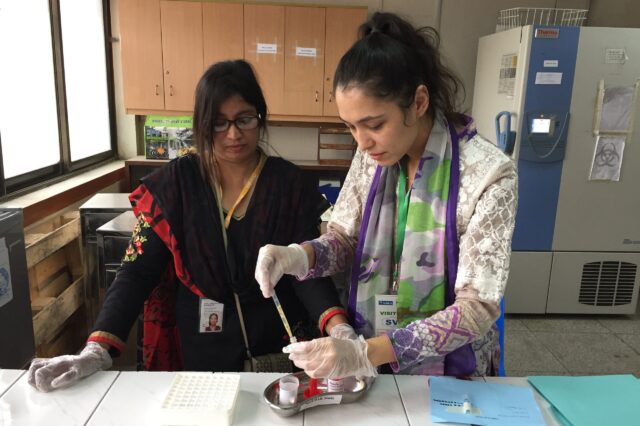
A study program coordinator demonstrates a stool culture to a local health worker in Dhaka, Bangladesh. (Photo courtesy of Adam C. Levine, M.D.)
For adults and older children, dehydration from diarrhea is a common, pervasive threat: Annually, more than 1 million die from it.
Now, a novel software tool that makes diagnosing and treating diarrhea-related dehydration faster, simpler and more accurate has been launched by an international team that includes a University of Florida Health pediatrics researcher.
The solution is as unique as the problem is massive. Worldwide, there are 5.7 billion cases of diarrhea a year among adults and older children. Even so, there has not been a convenient, easy-to-use, evidence-based tool for assessing dehydration in patients.
Seeing a large and urgent need, researchers at UF Health, Brown University and in Bangladesh teamed up to create FluidCalc. Using an algorithm that runs through a cell phone app, FluidCalc quickly and consistently determines the extent of a patient’s dehydration and calculates how much fluid they need. The tool uses two primary algorithms for those under and over 5 years of age.
“There’s a lot less left to chance if you have an evidence-based algorithm doing this instead of trying to determine each patient’s needs,” said Eric J. Nelson, M.D., Ph.D., an associate professor with UF’s College of Public Health and Health Professions and the UF College of Medicine’s department of pediatrics. Nelson’s contributions included developing the software that powers FluidCalc.
To evaluate the new algorithm among those over age 5, the researchers analyzed data from 1,580 people who were patients at the International Centre for Diarrhoeal Disease Research in Dhaka, Bangladesh. Patients were weighed on arrival and again every four hours. They were then assessed by two nurses using the digital tool and also established World Health Organization guidelines for dehydration severity.
FluidCalc outperformed the WHO algorithm at distinguishing severe dehydration from the absence of severe dehydration, the researchers found. The tool more accurately identified patients with severe dehydration as well as those without dehydration. The findings were published recently in the journal The Lancet Global Health.
FluidCalc is helpful to patients, doctors and other health care providers for several reasons, the researchers said. It reduces the chances of undertreating or overtreating diarrhea-related dehydration. Undertreating dehydration can cause shock or organ failure in patients, whereas overtreatment can lead to excess fluid in the lungs or brain. A consistent, simplified dehydration tool is also helpful to doctors, nurses and community health workers who are the first to assess patients. Diarrheal disease is the second leading cause of death globally for children between 1 month and 5 years of age.
“Getting dehydration assessment right is really important. And yet we have depended on clinicians to make this really important decision and make it billions of times every single year without giving them a good, accurate and reliable tool,” said Adam C. Levine, M.D., the associate dean of global health equity at Brown University and the study’s principal investigator.
Beyond patient care, accurate dehydration assessment has important implications for health care systems — especially in developing countries, Levine said. In some of those areas, intravenous fluids have to be imported and hospital beds can be scarce. Low-cost and effective oral rehydration solution is considered one of the most important life-saving health care innovations in history.
“If you can save those resources for the small percentage of patients who really need it because they have severe dehydration and then treat all of the other patients with much less expensive oral rehydration or nothing at all, it’s going to save a lot of money while getting the right care to patients and preserving lives,” Levine said.
Nelson, whose other worldwide work includes establishing an after-hours pediatric care and medicine delivery program in Haiti called MotoMeds, said FluidCalc’s value lies in its free, worldwide access and pinpoint accuracy in determining how much fluid a patient needs and whether it should be given intravenously or orally. The design of FluidCalc is now serving as a formative step for new National Institutes of Health-funded research led by Nelson to develop similar tools for other diseases. Those tools will be evaluated within MotoMeds’ clinical research infrastructure.
For FluidCalc, the researchers will further test the tool in Tanzania to determine its worldwide suitability without having to conduct trials in many individual countries. A longer-term goal is to get the WHO to change and update its guidelines for diarrhea-related dehydration, Levine said.
Scientists from Rhode Island Hospital and the International Centre for Diarrhoeal Research also contributed to the research. Funding for the research was provided by the National Institutes of Health’s National Institute for Diabetes and Digestive and Kidney Diseases.
About the author
