Congenital platelet function defects
Definition
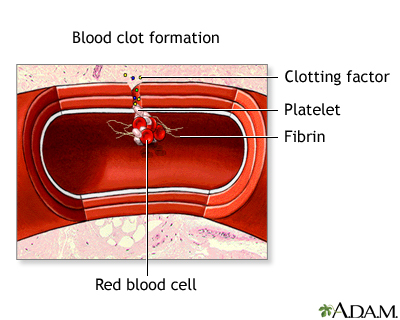
Congenital platelet function defects are conditions that prevent clotting elements in the blood, called platelets, from working as they should. Platelets help the blood clot. Congenital means present from birth.
Alternative Names
Platelet storage pool disorder; Glanzmann's thrombasthenia; Bernard-Soulier syndrome; Platelet function defects - congenital
Causes
Congenital platelet function defects are bleeding disorders that cause reduced platelet function.
Most of the time, people with these disorders have a family history of a bleeding disorder, such as:
- Bernard-Soulier syndrome occurs when platelets lack a substance that sticks to the walls of blood vessels. Platelets are typically large and of reduced number. This disorder may cause severe bleeding.
- Glanzmann thrombasthenia is a condition caused by the lack of a protein needed for platelets to clump together. Platelets are typically of normal size and number. This disorder may also cause severe bleeding.
- Platelet storage pool disorder (also called platelet secretion disorder) occurs when substances called granules inside platelets aren't stored or released properly. Granules help platelets function properly. This disorder causes easy bruising or bleeding.
Symptoms
Symptoms may include any of the following:
- Excessive bleeding during and after surgery
- Bleeding gums
- Easy bruising
- Heavy menstrual periods
- Nosebleeds
- Prolonged bleeding with small injuries
Exams and Tests
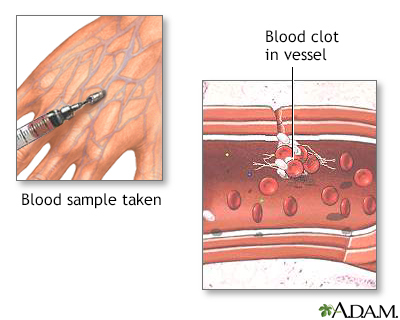
The following tests may be used to diagnose this condition:
- Complete blood count (CBC)
- Partial thromboplastin time (PTT)
- Platelet aggregation test
- Prothrombin time (PT)
- Platelet function analysis
- Flow cytometry
You may need other tests. Your relatives may need to be tested.
Treatment
There is no specific treatment for these disorders. However, your health care provider will likely monitor your condition.
You may also need:
- To avoid taking aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, because they can worsen bleeding symptoms.
- Platelet transfusions, such as during surgery or dental procedures.
Outlook (Prognosis)
There is no cure for congenital platelet function disorders. Most of the time, treatment can control the bleeding.
Possible Complications
Complications may include:
- Severe bleeding
- Iron deficiency anemia in menstruating women
When to Contact a Medical Professional
Call your provider if:
- You have bleeding or bruising and do not know the cause.
- Bleeding does not respond to the usual method of control.
Prevention
A blood test can detect the gene responsible for the platelet defect. You may wish to seek genetic counseling if you have a family history of this problem and are considering having children.
Gallery
References
Arnold DM, Zeller MP, Smith JW, Nazy I. Diseases of platelet number: immune thrombocytopenia, neonatal alloimmune thrombocytopenia, and posttransfusion purpura. In: Hoffman R, Benz EJ, Silberstein LE, et al, eds. Hematology: Basic Principles and Practice. 7th ed. Philadelphia, PA: Elsevier; 2018:chap 131.
Hall JE, Hall ME. Hemostasis and blood coagulation. In: Hall JE, Hall ME, eds. Guyton and Hall Textbook of Medical Physiology. 14th ed. Philadelphia, PA: Elsevier; 2021:chap 37.
Neff AT. Von Willebrand disease and hemorrhagic abnormalities of platelet and vascular function. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 164.