Gram-negative meningitis
Definition
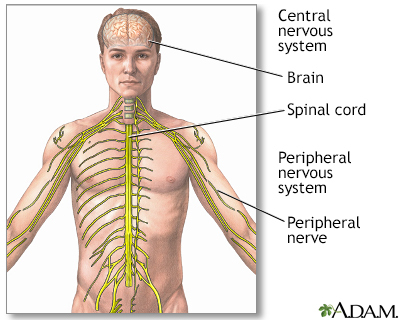
Meningitis is present when the membranes covering the brain and spinal cord become swollen and inflamed. This covering is called the meninges.
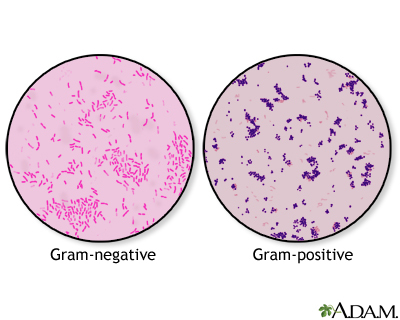
Bacteria are one type of germ that may cause meningitis. Gram-negative bacteria are a type of bacteria that behave in a similar manner in the body. They are called gram-negative because they turn pink when tested in the laboratory with a special stain called Gram stain.
Causes
Acute bacterial meningitis can be caused by different Gram-negative bacteria including meningococcus and H influenzae.
This article covers Gram-negative meningitis caused by the following bacteria:
- Escherichia coli
- Klebsiella pneumoniae
- Pseudomonas aeruginosa
- Serratia marcescens
Gram-negative meningitis is more common in infants than adults. But it can also occur in adults, especially those with one or more risk factors. Risk factors in adults and children include:
- Infection (especially in the abdomen or urinary tract)
- Recent brain surgery
- Recent injury to the head
- Spinal abnormalities
- Spinal fluid shunt placement after brain surgery
- Urinary tract abnormalities
- Urinary tract infection
- Weakened immune system
Symptoms
Symptoms usually come on quickly, and may include:
- Fever and chills
- Mental status changes
- Nausea and vomiting
- Sensitivity to light (photophobia)
- Severe headache
- Stiff neck (meningismus)
- Symptoms of a bladder, kidney, intestine, or lung infection
Other symptoms that can occur with this disease:
- Agitation
- Bulging fontanelles in infants
- Decreased consciousness
- Poor feeding or irritability in children
- Rapid breathing
- Unusual posture, with the head and neck arched backwards (opisthotonos)
Exams and Tests
The health care provider will perform a physical exam. Questions will focus on symptoms and possible exposure to someone who might have the same symptoms, such as a stiff neck and fever.
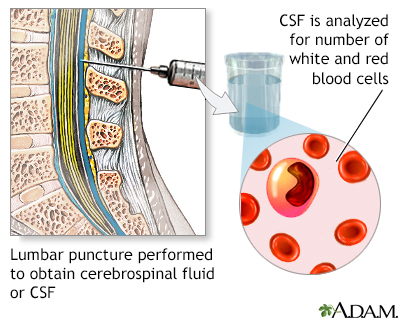
If the provider thinks meningitis is possible, a lumbar puncture (spinal tap) will likely be done to remove a sample of spinal fluid for testing.
Other tests that may be done include:
- Blood culture
- Chest x-ray
- CT scan of the head
- Gram stain or, other special stains, and culture of the spinal fluid
Treatment
Antibiotics will be started as soon as possible. Ceftriaxone, ceftazidime, and cefepime are the most commonly used antibiotics for this type of meningitis. Other antibiotics may be given, depending on the type of bacteria.
If you have a spinal shunt, it may be removed.
Outlook (Prognosis)
The earlier treatment is started, the better the outcome.
Many people recover completely. But, many people have permanent brain damage or die of this type of meningitis. Young children and adults over age 50 have the higher risk for death. How well you do depends on:
- Your age
- How soon treatment is started
- Your overall health
Possible Complications
Long-term complications may include:
- Brain damage
- Buildup of fluid between the skull and brain (subdural effusion)
- Buildup of fluid inside the skull that leads to brain swelling (hydrocephalus)
- Hearing loss
- Seizures
When to Contact a Medical Professional
Call 911 or the local emergency number or go to an emergency room if you suspect meningitis in a young child who has the following symptoms:
- Feeding problems
- High-pitched cry
- Irritability
- Persistent unexplained fever
Meningitis can quickly become a life-threatening illness.
Prevention
Prompt treatment of related infections may reduce the severity and complications of meningitis.
Gallery
References
Centers for Disease Control and Prevention website. Bacterial meningitis. www.cdc.gov/meningitis/bacterial.html. Reviewed July 15, 2021. Accessed November 10, 2022.
Nath A. Meningitis: bacterial, viral, and other. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 384.
Hasbun R, Van de Beek D, Brouwer MC, Tunkel AR. Acute meningitis. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 87.
