Laparoscopic Renal Cyst Ablation
Kidney cysts are a benign and fairly common condition that affects both men and women.
About 1 out of 4 people have a cyst on their kidney, and the majority of these cysts do not grow or cause problems throughout one’s lifetime. Occasionally, a renal cyst will continue to accumulate fluid over time, causing pain (Figure 1).
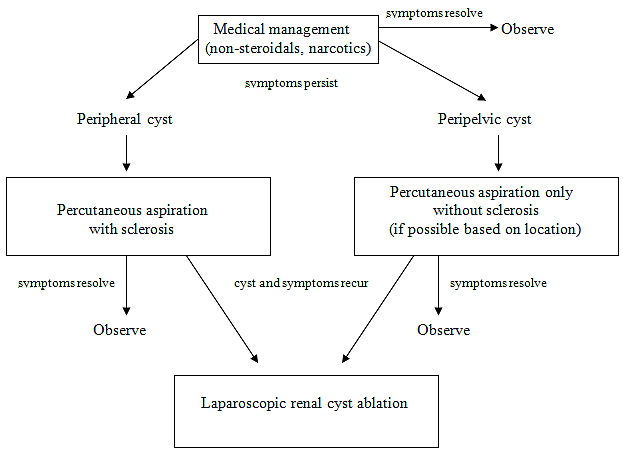
Most urologists treat these conservatively, either by observation, pain medication or by drainage through the skin with a needle by a radiologist. An algorithm of medical management for symptomatic renal cysts is shown in Figure 2.
Laparoscopic renal cyst ablation is an effective minimally invasive treatment for large, symptomatic kidney cysts especially those that recur despite needle aspiration/drainage.
The surgery
The operation
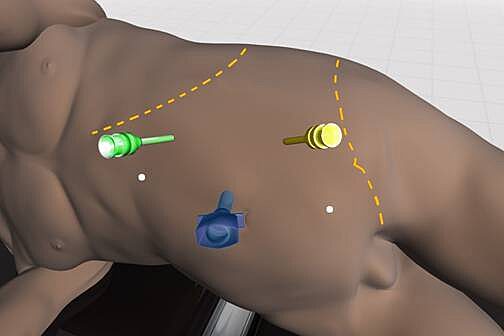
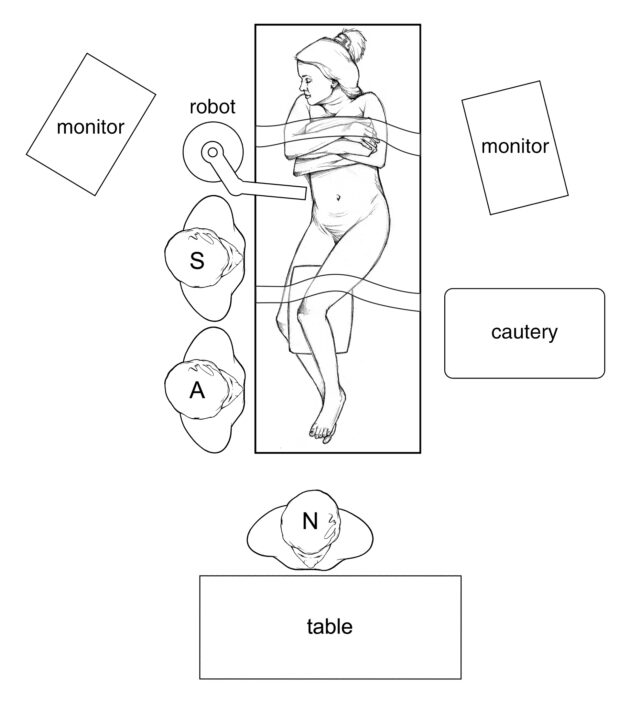
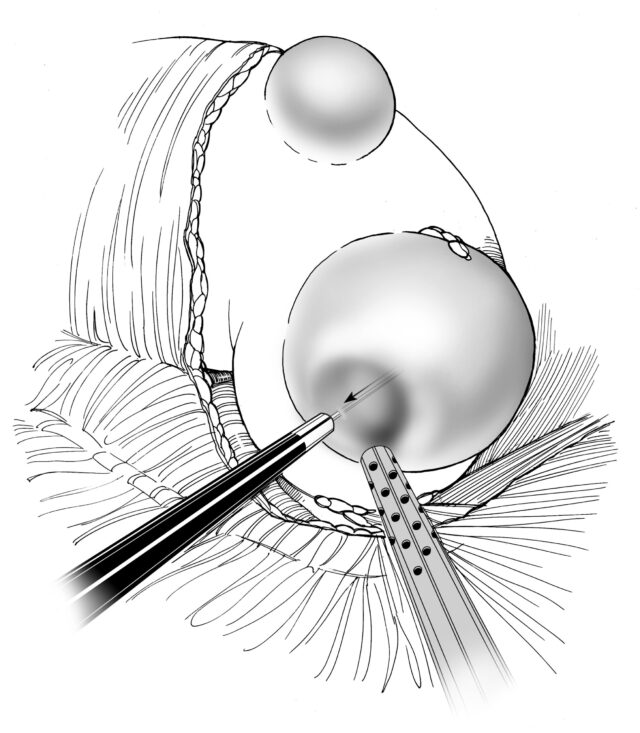
Laparoscopic renal cyst ablation requires that patients undergo a general anesthesia. While operative time varies from one individual to another, the average operating time is approximately 2-3 hours. Your surgeon will insert a telescope (called laparoscope) and surgical instruments through 3-4 small keyhole (<1 cm) incisions in the abdomen allowing him to inspect the internal organs and affected kidney (Figure 3).
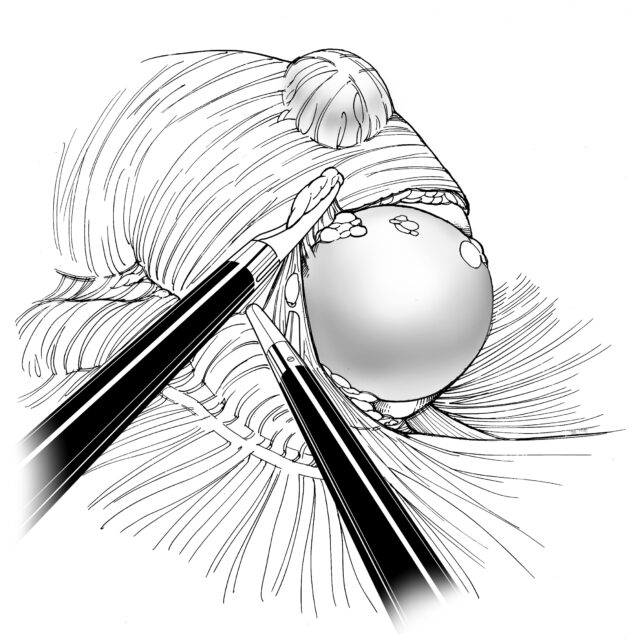
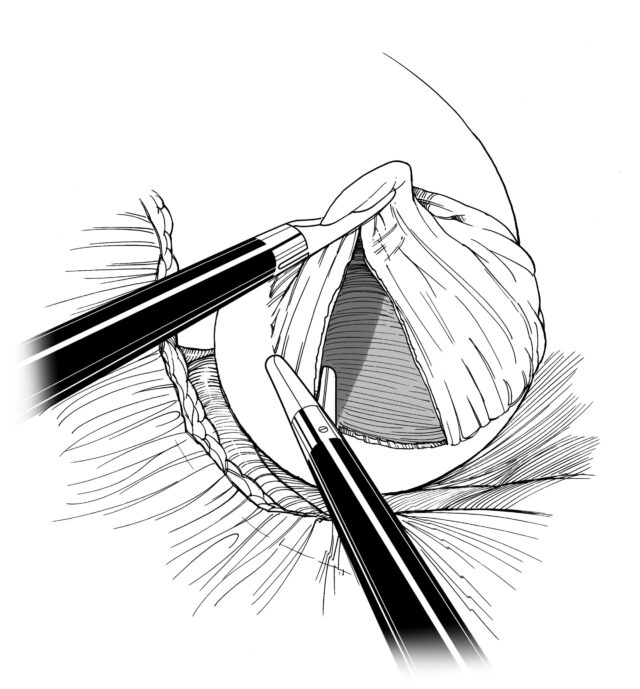
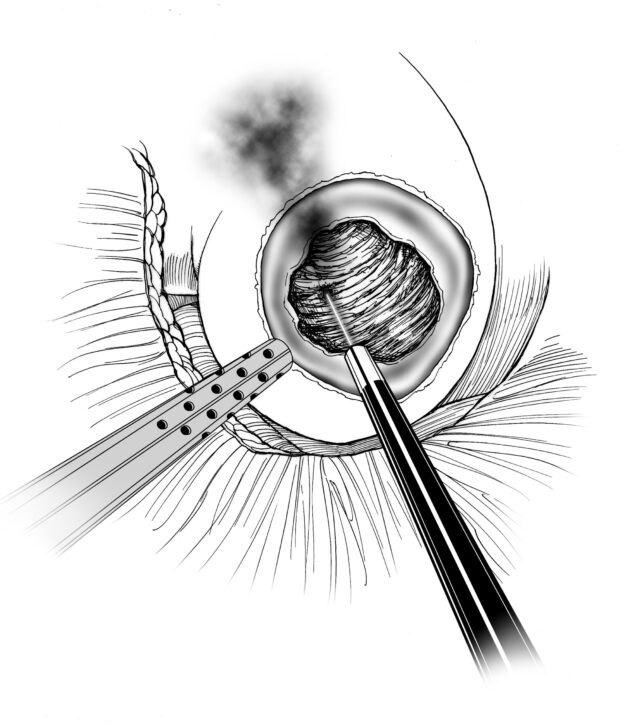
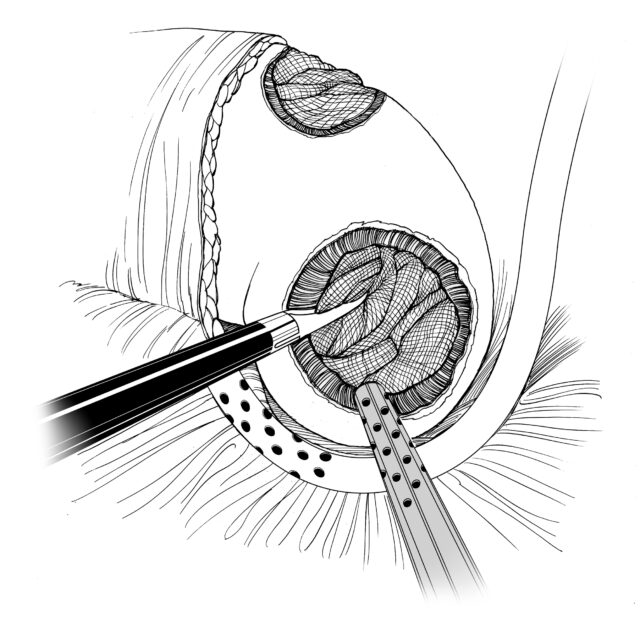
The abdomen is filled with carbon dioxide gas to create a larger working space for the surgeon to accomplish the operation. This gas is later evacuated from the abdomen at the conclusion of the operation. The kidney cyst is then isolated, drained and the wall of the cyst opened and excised using scissors. The removed portion of the cyst wall is sent to the pathologist for histologic analysis. The portion of the cyst directly on the kidney surface is coagulated to prevent fluid from being produced from the cyst lining. A drain is placed around the surgical site and is removed within 24-48 hours as long as no urine leak is detected. An internal ureteral stent is very rarely used.
Slideshow


Full length procedural video
Click to individual steps below
- Left Kidney Cyst
- Aspirating Cyst
- Excision of Cyst Wall
- Inspecting Renal Cyst
- Cauterization of Renal Cyst Wall
- Packing of Cyst Cavity with Absorbable Gauze
Potential risks and complications
As with any major surgery, complications, although rare, may occur with laparoscopic renal cyst ablation. Potential risks and complications with this operation include but are not limited to the following:
- Bleeding: Blood loss during this procedure is typically less than 100 cc with the rare need for a blood transfusion (<2% of patients). If you are interested in autologous blood transfusion (donating your own blood) prior to your surgery, you must make your surgeon aware. This can be arranged locally in Gainesville, FL at the Civitan Regional Blood center or at your local Red Cross.
- Infection: Although patients are given broad spectrum intravenous antibiotics immediately prior to surgery, infections of the urinary tract and skin incisions may still occur but are rare. If you develop any signs or symptoms of infection after the surgery (fever, drainage from or redness around your incisions, urinary frequency/discomfort, pain) please contact us at once.
- Cyst Recurrence: Although very effective, laparoscopic renal cyst ablation is associated with an approximately 5-10% chance of recurrence of the cyst.
- Persistent Pain: Some patients who undergo laparoscopic renal cyst ablation will continue to have chronic kidney pain despite resolution of the cyst by imaging.
- Urine Leak: When treating cyst that lie in close proximity to the drainage system of the kidney, any small entry into the drainage system can lead to a leakage of urine from the kidney into the surrounding tissues. Although rare, a urine leak may require ureteral stent and/or foley catheter placement to allow for spontaneous resolution of the leak.
- Adjacent Tissue / Organ Injury: Although uncommon, adjacent organs and tissues may be injured as a result of your surgery. This includes the colon, bowel, vascular structures, nerves, muscles, spleen, liver, pancreas and gallbladder. If injury to your lung cavity occurs, a small chest tube may be required to evacuate air, blood, and fluid from around your lung, thus allowing your lung to expand and work properly. On rare occasions, further surgery may be required to address unexpected injuries to adjacent organs.
- Complete Removal of Kidney: In very rare cases, circumstances may arise that may lead your surgeon to remove the entire kidney. These include excessive bleeding, or a tumor that appears within the kidney cysts that was not appreciated on preoperative imaging tests. In such cases, the kidney can generally be removed safely by laparoscopy and often does not require conversion to open surgery.
- Hernia: Because of the small laparoscopic incisions, hernias at these sites occur rarely. In addition, larger incisions are closed carefully prior to the completion of your surgery to minimize the risk of hernias.
- Conversion to Open Surgery: In the rare event of complications or due to difficulty in dissecting by means of laparoscopy surgery, conversion to open surgery is sometimes required. This could result in a larger standard open incision and possibly a longer recuperation period.
What to expect after surgery
Immediately after the surgery you will be taken to the recovery room then transferred to your hospital room once you are fully awake and alert.
- Postoperative Pain: Although most patients in the first few days after surgery experience mild pain at their incision sites, this is generally well controlled by use of intravenous pain medication, patient-controlled anesthesia pump, or oral pain medication provided by your nurse. You may experience some minor transient shoulder pain (1-2 days) related to the carbon dioxide gas used to inflate your abdomen during the laparoscopic or robotic surgery.
- Nausea: Nausea is common following any surgery especially related to general anesthesia. This is usually transient and controlled by medication which can be administered on an as needed basis by your nurse.
- Urinary Catheter: A urinary catheter (also called foley catheter) is placed to drain your bladder at the time of surgery while you are asleep. This is in efforts to monitor your urine output over the first day or so following surgery. This is generally removed by your nurse once you are walking comfortably. It is not uncommon to have blood-tinged urine for a few days after your surgery while your catheter is in place.
- Flank Drain: A small clear tube or drain will be placed during surgery exiting out of the side of your flank. The drain output will appear blood tinged but should be minimal. The drain primarily serves to identify any excessive bleeding or a urine leak from the cyst ablation site. The drain is typically removed on the day you are discharged from the hospital if the output remains low.
- Ureteral Stent: On rare occasions a small plastic, flexible tube called a ureteral stent will be placed at the time of your surgery to drain the kidney down towards the bladder. This is generally in cases where ablation of the cyst is in close proximity to the collecting system or drainage tract of your kidney and entry into the tract is suspected. The decision on whether to place a ureteral stent or not will be based upon each individual’s circumstance and the judgment of your surgeon. The stent serves to facilitate drainage of urine down to the bladder rather than out of the ablation site. At a later date, the stent will be removed in the office by your surgeon.
- Diet: Your diet will be advanced slowly following surgery from liquids to solids as tolerated. It is often the case that your appetite will be poor for up to a week following surgery. In addition, your intestinal function is often sluggish due to the effects of surgery and general anesthesia. It is for these two reasons that we recommend taking only small amounts of liquids by mouth at any one time until you begin to pass flatus and your appetite returns. In the meantime, your intravenous catheter will provide the necessary hydration to your body as you oral intake improves.
- Fatigue: Fatigue is quite common following surgery and should subside in a few weeks following surgery.
- Incentive Spirometry: You will be expected to do some very simple breathing exercises to help prevent respiratory infections through using an incentive spirometry device (these exercises will be explained to you by the nursing staff during your hospital stay). Coughing and deep breathing is an important part of your recuperation and helps prevent pneumonia and other pulmonary complications.
- Ambulation: On the evening of surgery it is very important to get out of bed and begin walking with the supervision of your nurse or family member to help prevent blood clots from forming in your legs. You can also expect to have SCD’s (sequential compression devices) wrapped around your lower legs and calf area to prevent blood clots called deep vein thrombosis from forming in your legs. In the days that follow surgery, patients are advised to walk at least 4-6 separate times a day in the hallways. This serves to further reduce the change of deep vein thrombosis and speed the return of bowel function.
- Constipation/Gas Cramps: You may experience sluggish bowels for several days following surgery as a result of the anesthesia. Suppositories and stool softeners are usually given to help with this problem. Taking a teaspoon of mineral oil daily at home will also help to prevent constipation. Narcotic pain medication can also cause constipation and therefore patients are encouraged to discontinue any narcotic pain medication as soon after surgery as tolerated.
- Hospital Stay: The length of hospital stay following laparoscopic renal cyst ablation is generally 1 day.
What to expect after discharge from the hospital
- Pain Control: For the majority of patients, one to two days of oral narcotic pain medication may be necessary after which Extra Strength Tylenol is usually sufficient to manage their pain. Again, narcotics should be minimized to avoid constipation and over sedation.
- Showering: Patients can shower immediately upon discharge from the hospital allowing their incisions to get wet. Once out of the shower, pad your incision sites dry and avoid any heavy creams or lotions. Tub baths or hot tubs in the first 2 weeks are discouraged as this will allow for prolonged soaking of your incisions and increase the risk of infection. You may shower after returning home from the hospital. Your wound sites can get wet, but must be patted dry immediately after showering. The adhesive tapes across your incisions, called Steri-strips, can be removed one week following surgery. The sutures underneath the skin will dissolve in 4-6 weeks.
- Activity: Walking 4-6 times a day for the first two weeks after surgery on a level surface is strongly encouraged as prolong sitting or lying can increase your risk of pneumonia and deep vein thrombosis. It is permissible to climb stairs. No heavy lifting or exertion for up to 4 weeks following surgery. Patients may begin driving once they are off of narcotic pain medication and have full range of motion at their waist. Most patients can return to full activity including work on an average 3-4 weeks after surgery.
- Diet: Patients may resume a regular diet as tolerated.
- Follow-up Appointment: Patients should make a follow-up appointment with their surgeon by contacting the UF Health Urology - Medical Plaza at (352) 265-8240. Your surgeon will let you know the timing and schedule of clinic visits following surgery.
- Pathology Results: The pathology results from your surgery are usually available in one week following surgery. Your results will be discussed with you either by phone or directly in the office during a follow-up clinic appointment.
Frequently asked questions (FAQs)
What is the advantage of laparoscopic renal cyst ablation as compared to open surgery?
Laparoscopic kidney surgery for treating symptomatic cysts have significant benefits to the patient including reduced blood loss and transfusions, reduced pain, shorter hospital stays, improved cosmesis, and a faster recovery as compared to open surgery. As such, it has become the standard of care for the surgical management of symptomatic, recurrent renal cysts. Published outcomes of laparoscopic renal cyst ablation appear comparable to open renal cyst ablation in terms resolution of the cyst and symptoms.
What is the overall success rate of laparoscopic renal cyst ablation?
Success rate in terms of complete radiographic resolution of the treated cyst is approximately 90% with symptomatic relief in approximately 95%.
Are there potential disadvantages?
In general there are no particular disadvantages; however, some situations may dictate the need for open surgery (see below).
What patients are not good candidates for laparoscopic renal cyst ablation?
Patients with a prior history of multiple and extensive abdominal surgery esp. kidney surgery may have excessive scarring around the kidney and cyst and therefore may not be ideal candidates for a laparoscopic approach. Patients with medical conditions such as severelung and heart disease may not be able to tolerate a laparoscopic approach due to the need for a general anesthetic.
What happens if complications arise and conversion to open surgery is required?
Although extremely rare, conversion to open surgery may be required if difficulty with dissection is encountered during the laparoscopic approach. Our surgeons are trained in open surgical approaches as well as laparoscopy and therefore are well equipped to complete the surgery in an open fashion if needed.