Definition
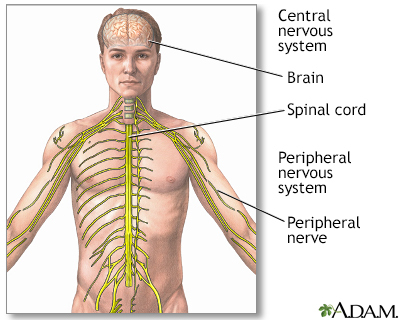
Meningitis is an infection of the membranes covering the brain and spinal cord. This covering is called the meninges.
Bacteria are one type of germ that can cause meningitis. The meningococcal bacteria are one kind of bacteria that cause meningitis.
Alternative Names
Gram negative - meningococcus
Causes
Meningococcal meningitis is caused by the bacteria Neisseria meningitidis (also known as meningococcus).
Meningococcus is the most common cause of bacterial meningitis in children and teens. It is a leading cause of bacterial meningitis in adults.
The infection occurs more often in winter or spring. It may cause local epidemics at boarding schools, college dormitories, or military bases.
Risk factors include recent exposure to someone with meningococcal meningitis, complement deficiency, use of eculizumab, spleen removal or a spleen that does not function, and exposure to cigarette smoking.
Symptoms
Symptoms usually come on quickly, and may include:
Fever and chills
Nausea and vomiting
Purple, bruise-like areas (
purpura)
Severe headache
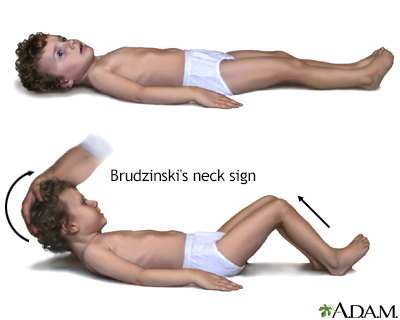
Stiff neck
Other symptoms that can occur with this disease:
- Agitation
- Bulging fontanelles in infants
- Decreased consciousness
- Poor feeding or irritability in children
- Rapid breathing
- Unusual posture with the head and neck arched backwards (opisthotonus)
Exams and Tests
The health care provider will perform a physical exam. Questions will focus on symptoms and possible exposure to someone who might have the same symptoms, such as a stiff neck and fever.
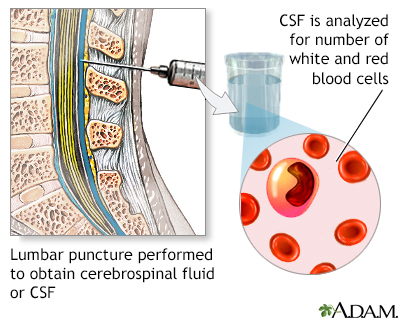
If the provider thinks meningitis is possible, a lumbar puncture (spinal tap) will likely be done to obtain a sample of spinal fluid for testing.
Other tests that may be done include:
Treatment
Antibiotics will be started as soon as possible.
- Ceftriaxone is one of the most commonly used antibiotics.
- Penicillin in high doses can be effective for susceptible bacteria.
- If there is an allergy to penicillin, chloramphenicol may be used.
Sometimes, corticosteroids may be given.
People in close contact with someone who have meningococcal meningitis should be given antibiotics to prevent infection.
Such people include:
- Household members
- Roommates in dormitories
- Military personnel who live in close quarters
- Those who come into close and long-term contact with an infected person
Outlook (Prognosis)
Early treatment improves the outcome. Death is possible. Young children and adults over age 50 have the highest risk of death.
Possible Complications
Long-term complications may include:
When to Contact a Medical Professional
Call 911 or the local emergency number or go to an emergency room if you suspect meningitis in a young child who has the following symptoms:
- Feeding difficulties
- High-pitched cry
- Irritability
- Persistent unexplained fever
Meningitis can quickly become a life-threatening illness.
Prevention
Close contacts in the same household, school, or day care center should be watched for early signs of the disease as soon as the first person is diagnosed. All family and close contacts of this person should begin antibiotic treatment as soon as possible to prevent spread of the infection. Ask your provider about this during the first visit.
Always use good hygiene habits, such as washing hands before and after changing a diaper or after using the toilet.
Vaccines for meningococcus are effective for controlling spread. They are currently recommended for:
- Adolescents
- College students in their first year living in dormitories
- Military recruits
- Travelers to certain parts of the world
Although rare, people who have been vaccinated can still develop the infection.
References
Centers for Disease Control and Prevention website. Bacterial meningitis. www.cdc.gov/meningitis/bacterial.html. Updated July 15, 2021. Accessed November 10, 2022.
Pollard AJ, Sadarangani M. Neisseria meningitides (meningococcus). In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 218.
Stephens DS. Neisseria meningitidis. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 211.