Definition
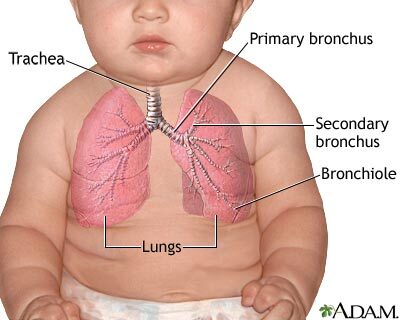
Babies with heart or lung problems may need to breathe increased amounts of oxygen to get normal levels of oxygen in their blood. Oxygen therapy provides babies with extra oxygen.
Alternative Names
Hypoxia - oxygen therapy in infants; Chronic lung disease - oxygen therapy in infants; BPD - oxygen therapy in infants; Bronchopulmonary dysplasia - oxygen therapy in infants
Information
Oxygen is a gas that the cells in your body need to work properly. The air we breathe normally contains 21% oxygen. We can receive up to 100% oxygen, which means that the gas being inhaled is pure oxygen.
HOW IS OXYGEN DELIVERED?
There are several ways to deliver oxygen to a baby. Which method is used depends on why and how much oxygen is needed and whether the baby needs a breathing machine. The baby must be able to breathe without assistance to use the first three types of oxygen therapy described below.
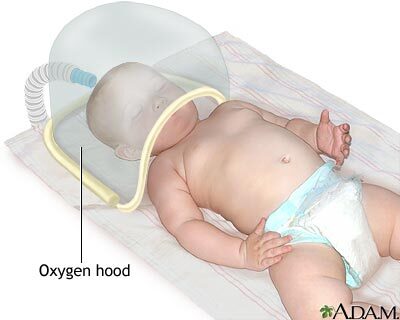
An oxygen hood or head box is used for babies who can breathe on their own but still need extra oxygen. A hood is a plastic dome or box with warm, moist oxygen inside. It often contains a device that measures the exact amount of oxygen the baby is receiving. The hood is placed over the baby's head to deliver oxygen.
A thin, soft, plastic tube called a nasal cannula may be used instead of a hood. This tube has soft prongs that gently fit into the baby's nose. Oxygen flows through the tube, but small amounts escape on the sides, so the amount of oxygen provided is not always received by the baby.
Another method is a nasal CPAP system. CPAP stands for continuous positive airway pressure. It is used for babies who need more help than they can get from an oxygen hood or nasal cannula, but who are still able to breathe on their own. Oxygen-containing air is delivered under higher pressure that helps the airways and lungs stay open ("inflated" or "expanded"). The air flows into the baby's nose through tubes attached to either soft nasal prongs or a small mask. Some oxygen can escape but generally less than with a nasal cannula because it's a tighter fit. CPAP is often used with premature babies who have trouble keeping their lungs inflated.
Finally, a breathing machine, or ventilator, may be needed to deliver increased oxygen and breathe for the baby. A ventilator can give extra pressure using the babies' own breaths, but can also deliver breaths to the baby if the baby is too weak, tired, or sick to breathe. In this case, the oxygen flows through a tube placed down the baby's windpipe. The baby usually receives close to the amount of oxygen being administered.
WHAT ARE THE RISKS OF OXYGEN?
Too much or too little oxygen can be harmful. If the cells in the body get too little oxygen, energy production decreases. With too little energy, cells may not work well and may die. Your baby may not grow properly. Many of the developing organs, including the brain and heart, may be injured.
Too much oxygen can also cause injury. Breathing too much oxygen can damage the lung. For babies who are born very prematurely, too much oxygen in the blood may also lead to problems in the brain and eye. Babies with certain heart conditions may also need lower levels of oxygen in the blood.
Your baby's health care providers will closely monitor and try to balance how much oxygen your baby needs. If you have questions about the risks and benefits of oxygen for your baby, discuss these with your baby's provider.
WHAT ARE THE RISKS OF OXYGEN DELIVERY SYSTEMS?
Infants receiving oxygen may get cold if the temperature of the oxygen is not warm enough. Because of this, it is often heated and humidified.
Some nasal cannulas use dry oxygen. At higher flow rates, this can irritate the inner nose, causing cracked skin, bleeding, or mucus plugs in the nose. This can increase the risk for infection.
Similar problems can occur with nasal CPAP devices. Also, some CPAP devices use wide nasal prongs that can cause skin breakdown around the nose if not fitted properly or if they shift while in use.
Mechanical ventilators have a number of risks as well. Your baby's providers will closely monitor and try to balance the risks and benefits of your baby's breathing support. If you have questions, discuss these with your baby's provider.
References
Bancalari E, Claure N, Jain D. Neonatal respiratory therapy. In: Gleason CA, Juul SE, eds. Avery's Diseases of the Newborn. 10th ed. Philadelphia, PA: Elsevier; 2018:chap 45.
Gregory DS. Resuscitation of the newborn. In: Kellerman RD, Rakel DP, Heidelbaugh JJ, Lee EM, eds. Conn's Current Therapy 2023. Philadelphia, PA: Elsevier 2023:1367-1373.
Vento M. Oxygen therapy in neonatal resuscitation. In: Martin RJ, Fanaroff AA, Walsh MC, eds. Fanaroff and Martin's Neonatal-Perinatal Medicine. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 33.