Peritonsillar abscess
Definition
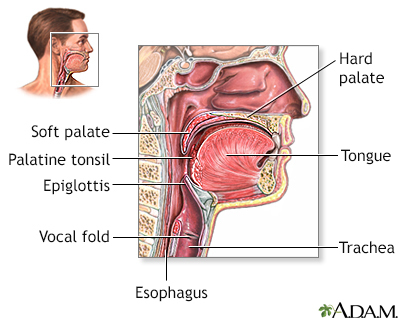
Peritonsillar abscess is a collection of infected material in the area around the tonsils.
Alternative Names
Quinsy; Abscess - peritonsillar; Tonsillitis - abscess
Causes
Peritonsillar abscess is a complication of tonsillitis. It is most often caused by a type of bacteria called group A beta-hemolytic streptococcus.
Peritonsillar abscess most often occurs in older children, adolescents, and young adults. The condition is rare now that antibiotics are used to treat tonsillitis.
Symptoms
One or both tonsils become infected. The infection may spread to the area around the tonsil. It can then spread down into the neck and chest. Swollen tissues can block the airway. This is a life-threatening medical emergency.
The abscess can break open (rupture) into the throat. The contents of the abscess can travel into the lungs and cause pneumonia.
Symptoms of peritonsillar abscess include:
- Fever and chills
- Severe throat pain that is usually on one side
- Ear pain on the side of the abscess
- Difficulty opening the mouth, and pain with opening the mouth
- Swallowing problems
- Drooling or inability to swallow saliva
- Facial or neck swelling
- Fever
- Headache
- Muffled voice
- Tender glands of the jaw and throat
- Neck stiffness
Exams and Tests
An exam of the throat often shows swelling on one side and on the roof of the mouth.
The uvula in the back of the throat may be shifted away from the swelling. The neck and throat may be red and swollen on one or both sides.
The following tests may be done:
- Aspiration of the abscess using a needle
- CT scan
- Fiber optic endoscopy to check if the airway is blocked
Treatment
The infection can be treated with antibiotics if it is caught early. If an abscess has developed, it will need to be drained with a needle or by cutting it open. You will be given pain medicine before this is done.
If the infection is very severe, the tonsils will be removed at the same time the abscess is drained, but this is rare. In this case, you will have general anesthesia so you will be asleep and pain-free.
Outlook (Prognosis)
In most cases, peritonsillar abscess goes away with treatment. The infection may return in the future.
Possible Complications
Complications may include:
- Airway obstruction
- Cellulitis of the jaw, neck, or chest
- Endocarditis (rare)
- Fluid around the lungs (pleural effusion)
- Inflammation around the heart (pericarditis)
- Pneumonia
- Sepsis (infection in the blood)
When to Contact a Medical Professional
Contact your health care provider right away if you have had tonsillitis and you develop symptoms of peritonsillar abscess.
Contact your provider if you have:
- Breathing problems
- Trouble swallowing
- Pain in the chest
- Persistent fever
- Symptoms that get worse
Prevention
Quick treatment of tonsillitis, especially if it is caused by bacteria, may help prevent this condition.
Gallery
References
Pappas DE, Hendley JO. Retropharyngeal abscess, lateral pharyngeal (parapharyngeal) abscess, and peritonsillar cellulitis/abscess. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 410.
Roginski MA, Atchinson PR. Upper respiratory tract infections. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 61.
Waage RK. Peritonsillar abscess drainage. In: Fowler GC, ed. Pfenninger and Fowler's Procedures for Primary Care. 4th ed. Philadelphia, PA: Elsevier; 2020:chap 206.
