Men’s Health Month: From Prostate Cancer Patient to Survivor and Advocate
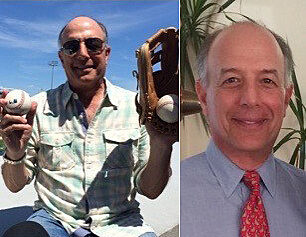
Tony Braun was at his urologist’s office one day in 2010 because of a kidney stone when the physician became alarmed. Bloodwork showed Tony’s prostate-specific…
Update your location to show providers, locations, and services closest to you.

The UF Health robotic prostatectomy is a minimally invasive surgical procedure for removing cancerous prostates in men. Utilizing an advanced robotic-assisted surgical system, University of Florida urologists specially trained in robotic surgeries perform small-incision prostate surgeries that deliver outstanding results.
The UF Health robotic prostatectomy is unique from other robotic programs in that it combines the most advanced robotic-assisted technology with UF surgeons fellowship-trained in robotic procedures and urology. Moreover, with the increased precision and control offered by the robotic device, UF surgeons are able to perform a specialized nerve-sparing procedure that was first performed and perfected by a UF urologist.
The UF Health robotic prostatectomy minimizes the risks of incontinence and impotence and offers qualified candidates many potential benefits over traditional prostatectomy surgery, including:
During the UF Health robotic prostatectomy surgeons carefully insert four tube-shaped robotic arms -- each about the diameter of a dime -- into separate small incisions in the patient's abdomen. The arms are equipped with lights, a stereoscopic camera that allows the surgeon and surgical team unprecedented three-dimensional viewing of the procedure, and specialized laparoscopic surgical instruments that respond precisely to every movement of the surgeon's hands.
Surgeons then perform a robotic-assisted hydro dissection of the prostate nerve bundles -- a specialized nerve-sparing procedure only performed at UF Health Shands Hospital --that improves post-operative urinary continence and potency.
In addition to avoiding major incisions and damage to surrounding muscle and tissue, the UF Health robotic prostatectomy allows surgeons greater visualization, dexterity, precision, control and superior ergonomics than during laparoscopic surgery.
Learn more about the UF department of urology by visiting the department website: http://www.urology.ufl.edu.
For more information about the UF Health robotic prostatectomy at UF Health Shands Hospital, please call
1-855-4UF-HEALTH .

David A. Cofrin Professor of Urology
Associate Chairman of Clinical Affairs and Director of Robotic and Minimally Invasive Urologic Surgery
Dr. Su received his medical degree from Weill-Cornell Medical College in New York, NY in 1994 and urology residency at New York Presbyterian Hospital-Cornell in 2000. He then completed a fellowship in laparoscopy, robotics and minimally invasive urologic surgery in 2001 at Johns Hopkins University, where he remained on staff for eight years, serving as the Director of Minimally Invasive Urologic Surgery from 2006-2008.
Dr. Su joined the urology department at the University of Florida in July 2008 as the David A. Cofrin Endowed Professor of Urology and Director of Robotic and Minimally Invasive Urologic Surgery. His clinical interests include robotic prostatectomy using the daVinci Surgical Robotic System for treating prostate cancer and laparoscopic partial nephrectomy for treating kidney cancer. He has performed more than 600 laparoscopic and robotic prostatectomies and more than 200 laparoscopic kidney surgeries. His research interests include augmented reality for soft tissue intraoperative navigation and imaged-based technologies as applied to urologic surgery.

UF Assistant Professor of Urology
Dr. Canales came to the University of Florida in 2007 after completing a fellowship in stone disease, laparoscopy and robotics. During his fellowship, he was designated an American Urological Association Foundation Research Scholar and received funding to study the protein pathways involved in kidney stone formation. His team's discovery of over ninety previously unreported proteins contained with kidney stone matrix has received two separate laboratory science research awards, including first place in the Prize Essay Contest awarded at the 2008 Annual AUA meeting and second place in the 2007 Endourological Society Fellow Essay contest. Most recently, he has teamed with Dr. Saeed Khan, an internationally recognized leader in stone disease research at the University of Florida, and has received a NIH grant to better define the role of calcium phosphate in the early phases of kidney stone development.
Dr. Canales' clinical interest is in the treatment of patients with metabolic stone disease, including percutaneous nephrolithotomy, ureteroscopy, and shock wave lithotripsy. In addition, Dr. Canales focuses on minimally invasive management of renal tumors and obstruction, including laparoscopic approaches to nephrectomy, partial nephrectomy, cryoablation, and pyeloplasty. He has authored over 30 peer reviewed manuscripts, multiple abstracts and book chapters, and is considered a leader in the area of proteomics and urologic stone disease.
UF Assistant Professor of Urology and Medical Director of the Urologic Quality and Safety Program
Dr. Gilbert is an Assistant Professor in the Department of Urology at the University of Florida with a joint appointment in the Department of Epidemiology and Health Policy Research. He specializes in the surgical management of urologic cancers, including prostate, bladder, kidney and testis cancer. Dr. Gilbert's clinical practice includes both early-stage and advanced cancers, and he uses both tradition (open surgery) and laparoscopic robot-assisted approaches according to clinical circumstances.
Dr. Gilbert's research focuses on surgical quality, cancer survivorship, and understanding ways in which cancer care and outcomes can be improved. He has authored 30 peer reviewed manuscripts in the area of urologic oncology and cancer survivorship, and has received several awards for his research.

UF Associate Professor of Urology, Director of Clinical Research
Dr. Dahm received his medical degree from the University of Heidelberg in Germany before completing his residency at Duke University in North Carolina, where he served both as senior and chief resident in the division of urology.
Prior to moving to Gainesville, where he practices at UF Health Shands Hospital, Shands AGH and the Veteran's Administration Medical Center, Dr. Dahm was an assistant professor of urology in the department of surgery at Duke University Medical Center, as well as an attending physician at the Veterans Administration Medical Center in Durham.
Dr. Dahm's clinical specialties and interests include urologic oncology, prostate cancer, immunotherapy, research methodology and evidence-based medicine.
For more information about the surgeons, visit the UF department of urology Web site at http://urology.ufl.edu. To schedule an appointment, please call the UF Health Shands Consultation Center at 352.265.0943.

The UF Health robotic prostatectomy is powered by the state-of-the-art da Vinci ® S-series Surgical System, which allows a surgeon's hand movements to be scaled, filtered and translated into precise movements of micro-instruments within the operative site. The magnified, three-dimensional view the surgeons experience on the high definition monitors enables them to perform precise surgery in complex procedures through small surgical incisions.
The da Vinci ® System enhances surgical capabilities by enabling the performance of complex surgeries through tiny surgical openings. The robotic system cannot be programmed, nor can it make decisions on its own, and requires that every surgical maneuver be performed with direct input from the surgeon.
The da Vinci® Surgical System has been successfully used in thousands of prostate cancer procedures world-wide.
For additional information on the da Vinci® Surgical System, visit http://davinciprostatectomy.com.

Tony Braun was at his urologist’s office one day in 2010 because of a kidney stone when the physician became alarmed. Bloodwork showed Tony’s prostate-specific…
Travis Rockey, 67, and Gail, his wife of 43 years, spend their days in retirement serving others. "We believe that service to others is a critical part of…
