Patient education
Definition
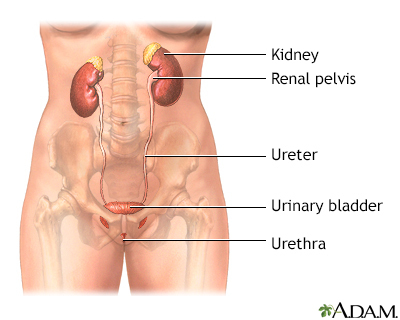
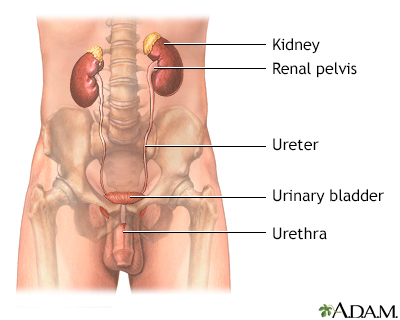
Urinary (or bladder) incontinence occurs when you are not able to keep urine from leaking out of your urethra. The urethra is the tube that carries urine out of your body from your bladder. You may leak urine from time to time. Or, you may not be able to hold any urine.
Urinary Incontinence Quiz
The three main types of urinary incontinence are:
- Stress incontinence -- occurs during activities like coughing, sneezing, laughing, or exercise.
- Urge incontinence -- occurs as a result of a strong, sudden need to urinate immediately. Then the bladder squeezes and you lose urine. You don't have enough time after you feel the need to urinate to get to the bathroom before you do urinate.
- Overflow incontinence -- occurs when the bladder does not empty and the volume of urine exceeds its capacity. This leads to dribbling.
Mixed incontinence occurs when you have more than one type of incontinence, usually both stress and urge urinary incontinence.
Bowel incontinence is when you are unable to control the passage of stool. It is not covered in this article.
Alternative Names
Loss of bladder control; Uncontrollable urination; Urination - uncontrollable; Incontinence - urinary; Overactive bladder
Causes
Causes of urinary incontinence include:
- Blockage in the urinary system
- Brain or nerve problems
- Dementia or other mental health problems that make it hard to feel and respond to the urge to urinate
- Problems with the urinary system
- Nerve and muscle problems
- Weakness of the pelvic or urethral muscles
- Enlarged prostate
- Diabetes
- Use of certain medicines
Incontinence may be sudden and go away after a short period of time. Or, it may continue long-term. Causes of sudden or temporary incontinence include:
- Bedrest -- such as when you are recovering from surgery
- Certain medicines (such as diuretics, antidepressants, tranquilizers, some cough and cold remedies, and antihistamines)
- Mental confusion
- Pregnancy
- Prostate infection or inflammation
- Stool impaction from severe constipation, which causes pressure on the bladder
- Urinary tract infection or inflammation
- Weight gain
Causes that may be more long-term include:
- Alzheimer disease.
- Bladder cancer.
- Bladder spasms.
- Large prostate in men.
- Nervous system conditions, such as multiple sclerosis or stroke.
- Nerve or muscle damage after radiation treatment to the pelvis.
- Pelvic prolapse in women which is falling or sliding of the bladder, urethra, or rectum into the vagina. This may be caused by pregnancy and delivery.
- Problems with the urinary tract.
- Spinal cord injuries.
- Weakness of the sphincter, the circle-shaped muscles that open and close the bladder. This can be caused by prostate surgery in men, or surgery to the vagina in women.
Home Care
If you have symptoms of incontinence, see your health care provider for evaluation, tests, and a treatment plan. Which treatment you get depends on what caused your incontinence and what type you have.
There are several treatment approaches for urinary incontinence:
Lifestyle changes. These changes may help improve incontinence. You may need to make these changes along with other treatments.
- Keep your bowel movements regular to avoid constipation. Try increasing the fiber in your diet.
- Quit smoking to reduce coughing and bladder irritation. Smoking also increases your risk for bladder cancer.
- Avoid alcohol and caffeinated drinks such as coffee, which can stimulate your bladder.
- Lose weight if you need to.
- Avoid foods and drinks that may irritate your bladder. These include spicy foods, carbonated drinks, and citrus fruits and juices.
- If you have diabetes, keep your blood sugar under good control.
For urine leaks, wear absorbent pads or undergarments. There are many well-designed products that no one else will notice.
Bladder training and pelvic floor exercises. Bladder retraining helps you gain better control over your bladder. Kegel exercises can help strengthen the muscles of your pelvic floor. Your provider can show you how to do them. Many women do not do these exercises correctly, even if they believe they are doing them correctly. Often, people benefit from formal bladder strengthening and retraining with a pelvic floor specialist.
Medicines. Depending on the type of incontinence you have, your provider may prescribe one or more medicines. These medicines help prevent bladder muscle spasms, relax the bladder, and improve bladder function. Your provider can help you learn how to take these medicines and manage their side effects.
Surgery. If other treatments do not work, or you have severe incontinence, your provider may recommend surgery. The type of surgery you have will depend on:
- The type of incontinence you have (such as urge, stress, or overflow)
- The severity of your symptoms
- The cause (such as pelvic prolapse, enlarged prostate, enlarged uterus, or other causes)
If you have overflow incontinence or you cannot fully empty your bladder, you may need to use a catheter. You may use a catheter that stays in long-term, or one that you are taught to put in and take out yourself.
Bladder nerve stimulation. Urge incontinence and urinary frequency can sometimes be treated by electrical nerve stimulation. Pulses of electricity are used to reprogram bladder reflexes. In one technique, the provider inserts a stimulator through the skin near a nerve in the leg. This is done weekly in the provider's office. Another method uses battery-operated implanted device similar to a pacemaker that is placed under the skin in the lower back.
Botox injections. Urge incontinence can sometimes be treated with an injection of onabotulinum A toxin (also known as Botox). The injection relaxes the bladder muscle and increases the storage capacity of the bladder. The injection is delivered through a thin tube with a camera on the end (cystoscope). In most cases, the procedure can be done in the provider's office.
When to Contact a Medical Professional
Talk to your provider about incontinence. Some providers who treat incontinence are gynecologists and urologists that specialize in this problem. They can find the cause and recommend treatments.
Call your local emergency number (such as 911) or go to an emergency room if you suddenly lose control over urine and you have:
- Difficulty talking, walking, or speaking
- Sudden weakness, numbness, or tingling in an arm or leg
- Loss of vision
- Loss of consciousness or confusion
- Loss of bowel control
Contact your provider if you have:
- Cloudy or bloody urine
- Dribbling
- Frequent or urgent need to urinate
- Pain or burning when you urinate
- Trouble starting your urine flow
- Fever
Gallery
References
Heesakkers JPFA, Blok B. Electrical stimulation and neuromodulation in storage and emptying failure. In: Partin AW, Dmochowski RR, Kavoussi LR , Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 122.
Lentz GM, Miller JL. Lower urinary tract function and disorders: physiology of micturition, voiding dysfunction, urinary incontinence, urinary tract infections, and painful bladder syndrome. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 21.
Newman DK, Burgio KL. Conservative management of urinary incontinence: behavioral and pelvic floor therapy, urethral and pelvic devices. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 121.
Resnick NM. Incontinence. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 23.
Reynolds WS, Dmochowski R, Karram MM, Mahdy A. Surgical management of refractory overactive bladder and detrusor compliance abnormalities. In: Baggish MS, Karram MM, eds. Atlas of Pelvic Anatomy and Gynecologic Surgery. 5th ed. Philadelphia, PA: Elsevier; 2021:chap 90.
Related conditions & treatments
Related specialties
Aftercare and more
- Indwelling catheter care
- Kegel exercises - self-care
- Multiple sclerosis - discharge
- Prostate resection - minimally invasive - discharge
- Radical prostatectomy - discharge
- Self catheterization - female
- Self catheterization - male
- Sterile technique
- Transurethral resection of the prostate - discharge
- Urinary catheters - what to ask your doctor
- Urinary incontinence - what to ask your doctor
- Urinary incontinence products - self-care
- Urinary incontinence surgery - female - discharge
- Urine drainage bags
- When you have urinary incontinence