Bystander CPR Helps Michael Overcome Sudden Cardiac Arrest
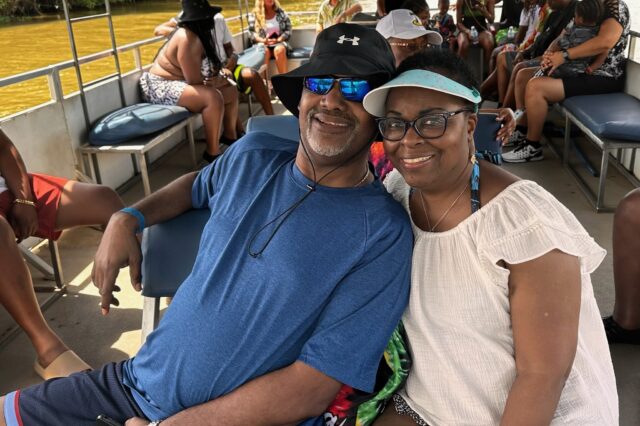
Sitting in church and practicing songs for Sunday service, Valerie Layton unexpectedly felt the weight of her husband Michael lean on her. It was April 1, so she thought he might be playing a joke on her.
But Michael, 63, was unconscious and had no pulse. He had experienced sudden cardiac arrest and needed immediate medical attention.
“Everything was normal. No complaints, chest pain, tiredness, palpitations. Nothing,” Valerie said. “Me and one other friend got him to the floor and started CPR because he wasn’t responsive. CPR was initiated and soon several friends who had been in a different room descended and immediately joined in the resuscitation efforts.”
Valerie, a physician assistant in the University of Florida Department of Neurosurgery, never imagined she’d need to perform CPR on her husband. Yet here she was, on a normal Saturday afternoon at Cross Point Church of God on Northwest 34th Street, but she was surrounded by several people from her community who sprang into action to help with CPR with Gainesville Fire Rescue on the way.
In that short but nerve-racking time, Valerie was left with an image that she says no movie or TV show could fully capture.
“A couple of times he took a deep gasp, but other than that, he looked gone,” Valerie said. “His eyes were kind of half open, but he was staring, and his eyes weren’t moving at all. He was just staring but not seeing anything. He threw up one time. It was really scary.”
Fortunately, the quick help she got from bystanders in the church who helped administer CPR before fire rescue came allowed Michael to receive blood to his brain and organs despite being unconscious.
Once on the scene, fire rescue personnel took an alternate route to deliver IV fluids and medication by opening a hole in his kneecap with a tool that Valerie described as “basically like a drill bit from Lowe’s.” This intraosseous (IO) infusion technique allows victims to receive fluids faster than if rescuers had to locate a suitable vein.
More CPR and defibrillator shocks weren’t enough to achieve a life-sustaining heart rhythm, so fire rescue transported Michael to UF Health’s cardiac intensive care unit to get the care he needed. After about 30 minutes of being unconscious, Michael opened his eyes and was surprised to see himself in a hospital bed surrounded by anxious loved ones.
“The first person I saw was my wife. She was standing right next to the bed,” Michael said. “I asked her, ‘What’s going on?’ I saw a whole bunch of people and a bunch of voices. I didn’t know what was going on. She said I passed out, and I said, ‘What??’ And I got very sad at that point. It was just taken from my memory.”
The last thing Michael could recall was the first song they had sung at church. When he regained his faculties, he realized he had been in the fight of his life. At one point, his ejection fraction — the percentage of the total amount of blood in your heart that is pumped out with each heartbeat — was at a dangerously low 10%. A normal EF is 50% or higher.
Still, despite the odds, somehow everything lined up perfectly to keep him alive. Michael could’ve suffered cardiac arrest while driving or even just standing or simply been in a place where bystander CPR wasn’t available. How things unfolded makes Michael believe that “if God wasn’t present, we wouldn’t be having this conversation right now.”
“The way that it played out, it could’ve been one of those scenarios where she left and went to church, and I’m home by myself, and she would’ve come and found my cold body because I would’ve been gone.”
The cause of his cardiac arrest is still unknown, and Michael was diagnosed with nonischemic cardiomyopathy. After four days in the hospital, UF Health’s Michael Massoomi, MD, an assistant professor in the UF Division of Cardiovascular Medicine, performed surgery on Michael to install an internal defibrillator under his skin that also acts as a pacemaker. The device, which can be seen as a small lump in his chest, is wired to his heart for the rest of his life. He can also monitor his heart from an app on his cell phone.
The couple says they’ll advocate for CPR training at their church and to install an automatic external defibrillator, or AED. The unpredictable nature of Michael’s case is a textbook example of why everyone should learn CPR.
“Events like this happen out of the blue. You can’t predict them,” Valerie said. “He hadn’t shown any signs that his heart was going to give out so I think it’s good to know it could happen to someone you love. It’s something that’s easy to do and can have lifelong effects for people who need it.”
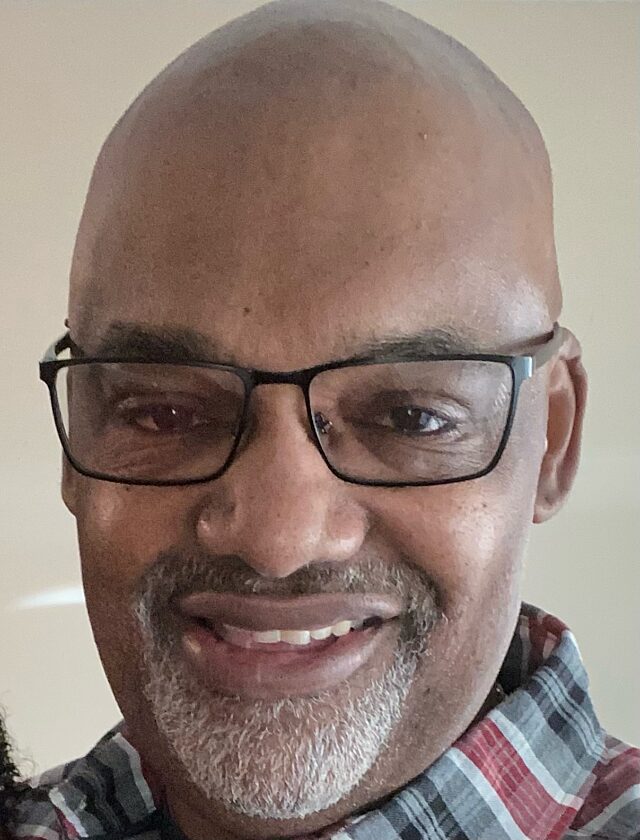
— Michael Layton
Michael can attest to the importance of CPR and the treatment he received at UF Health that followed.
“Everybody was about the business,” said Michael, who will have a follow-up appointment with a UF Health electrophysiologist in July. “The doctors, the nurses, the cleaning people, the people delivering the food, the team of cardiologists. Every single one of them was spot-on.”
Resources
Hands-only CPR is CPR without mouth-to-mouth breaths, and it has been shown to be as effective as conventional CPR for cardiac arrest, doubling or even tripling a victim’s chance of survival.
PulsePoint Respond is a free mobile app that alerts all potential first-responders — including citizens and off-duty medical professionals — who are within a quarter-mile of the person experiencing a cardiac arrest. The app provides directions on where to find the person in need, then displays reminders on how to deliver chest compressions.
About the author