The Importance of Colorectal Cancer Screening: How Early Detection Saves Lives
Colorectal cancer ranks as the second leading cause of cancer-related deaths in the United States. Referred to as a “silent killer” due to its lack of…

Update your location to show providers, locations, and services closest to you.
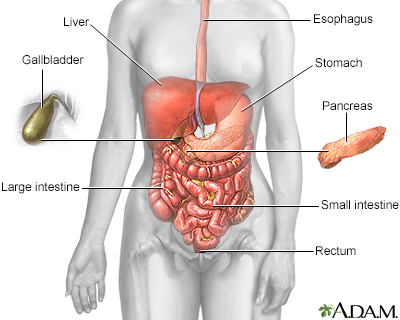
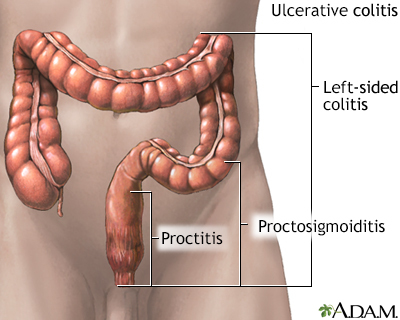
Ulcerative colitis is a condition in which the lining of the large intestine (colon) and rectum become inflamed. It is a form of inflammatory bowel disease (IBD). Crohn disease is a related condition.
Inflammatory bowel disease - ulcerative colitis; IBD - ulcerative colitis; Colitis; Proctitis; Ulcerative proctitis
The cause of ulcerative colitis is unknown. People with this condition have problems with their immune system. However, it is not clear if immune problems cause this illness. Stress and certain foods can trigger symptoms, but they do not cause ulcerative colitis.
Ulcerative colitis may affect any age group. There are peaks at ages 15 to 30 and then again at ages 50 to 70.
The disease begins in the rectal area. It may stay in the rectum or spread to higher areas of the large intestine. However, the disease does not skip areas. It may involve the entire large intestine over time.
Risk factors include a family history of ulcerative colitis or other autoimmune diseases, or Jewish ancestry.
The symptoms can be more or less severe. They may start slowly or suddenly. Half of people only have mild symptoms. Others have more severe attacks that occur more often. Many factors can lead to attacks.
Symptoms may include:
Children's growth may slow.
Other symptoms that may occur with ulcerative colitis include the following:
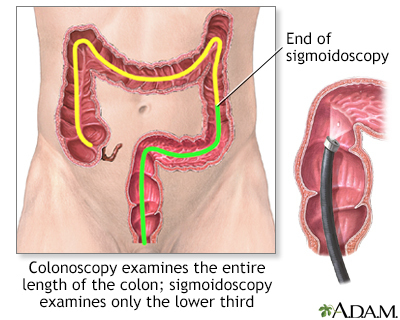
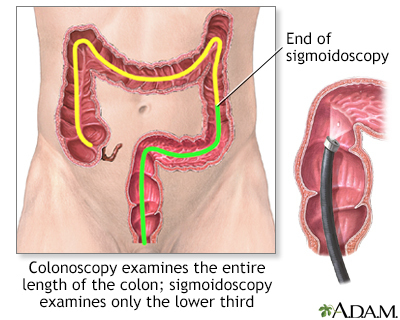
Colonoscopy with biopsy is most often used to diagnose ulcerative colitis. Colonoscopy is also used to screen people with ulcerative colitis for colon cancer.
Other tests that may be done to help diagnose this condition include:
Sometimes, tests of the small intestine are needed to differentiate between ulcerative colitis and Crohn disease, including:
The goals of treatment are to:
During a severe episode, you may need to be treated in the hospital. Your doctor may prescribe corticosteroids. You may be given nutrients through a vein (IV line).
DIET AND NUTRITION
Certain types of foods may worsen diarrhea and gas symptoms. This problem may be more severe during times of active disease. Diet suggestions include:
STRESS
You may feel worried, embarrassed, or even sad or depressed about having a bowel accident. Other stressful events in your life, such as moving, or losing a job or a loved one can cause worsening of digestive problems.
Ask your health care provider for tips about how to manage your stress.
MEDICINES
Medicines that may be used to decrease the number of attacks include:
SURGERY
Surgery to remove the colon will cure ulcerative colitis and removes the threat of colon cancer. You may need surgery if you have:
Most of the time, the entire colon, including the rectum, is removed. After surgery, you may have:
Social support can often help with the stress of dealing with illness, and support group members may also have useful tips for finding the best treatment and coping with the condition.
The Crohn's and Colitis Foundation of America (CCFA) has information and links to support groups.
Symptoms are mild in about one half of people with ulcerative colitis. More severe symptoms are less likely to respond well to medicines.
Cure is only possible through complete removal of the large intestine.
The risk for colon cancer increases in each decade after ulcerative colitis is diagnosed.
You have a higher risk for small bowel and colon cancer if you have ulcerative colitis. At some point, your provider will recommend tests to screen for colon cancer.
More severe episodes that recur may cause the walls of the intestines to become thickened, leading to:
Problems absorbing nutrients may lead to:
Less common problems that may occur include:
Contact your provider if:
There is no known prevention for this condition.
Goldblum JR, Large bowel. In: Goldblum JR, Lamps LW, McKenney JK, Myers JL, eds. Rosai and Ackerman's Surgical Pathology. 11th ed. Philadelphia, PA: Elsevier; 2018:chap 17.
Lichtenstein GR. Inflammatory bowel disease. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 132.
Mowat C, Cole A, Windsor A, et al. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2011;60(5):571-607. PMID: 21464096 pubmed.ncbi.nlm.nih.gov/21464096/.
Rubin DT, Ananthakrishnan AN, Siegel CA, Sauer BG, Long MD. ACG clinical guidelines: ulcerative colitis in adults. Am J Gastroenterol. 2019:114(3):384-413. PMID: 30840605 pubmed.ncbi.nlm.nih.gov/30840605/.
Ungaro R, Mehandru S, Allen PB, Peyrin-Biroulet L, Colombel JF. Ulcerative colitis. Lancet. 2017;389(10080):1756-1770. PMID: 27914657 pubmed.ncbi.nlm.nih.gov/27914657/.
Our community and patient programs provide great value to patients, families and loved ones. People can find support, educational materials, expert consultants and more. In most instances, these programs are offered free of charge.
Support system for those students with inflammatory bowel disease.
Colorectal cancer ranks as the second leading cause of cancer-related deaths in the United States. Referred to as a “silent killer” due to its lack of…

Ask Ethan Church what he’s passionate about and the answer may seem unusual for a 17-year-old: forestry and soil science. A first-degree black belt assistant…
